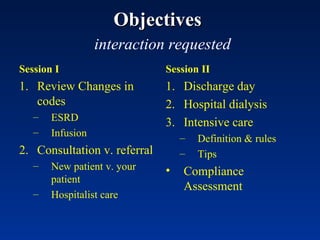
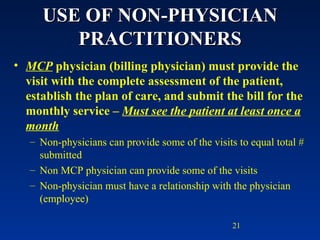
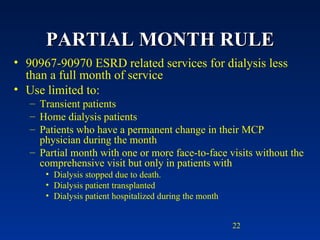
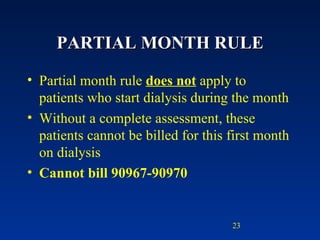
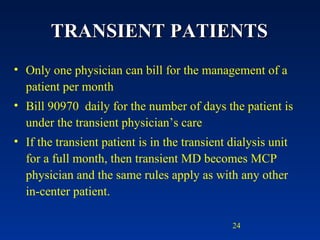
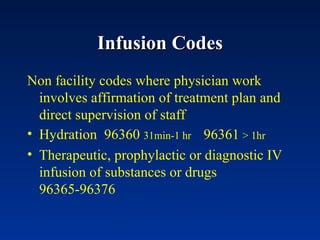
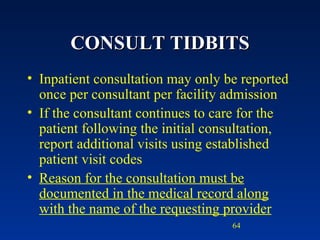
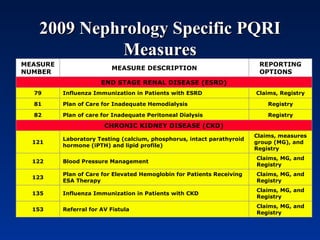
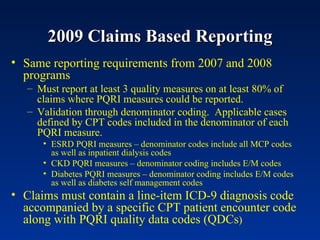
The document provides guidance on coding and billing for end-stage renal disease (ESRD) services. It discusses:
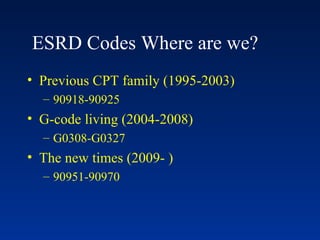
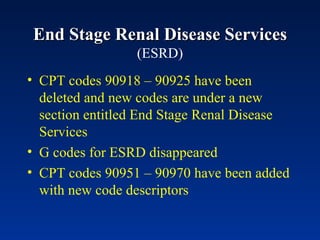
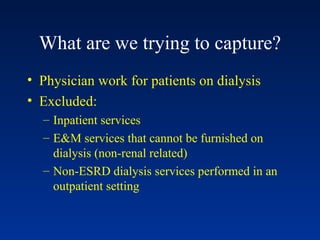
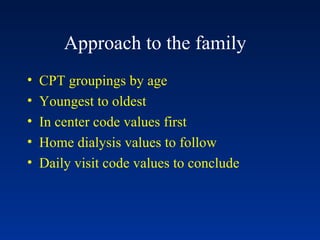
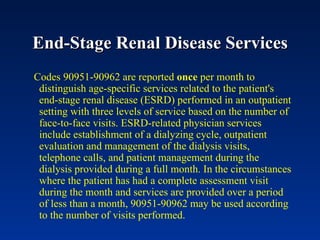
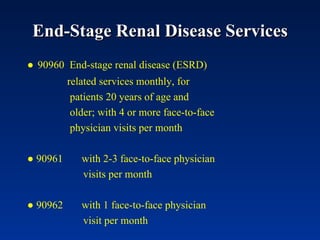
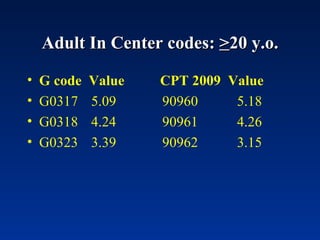
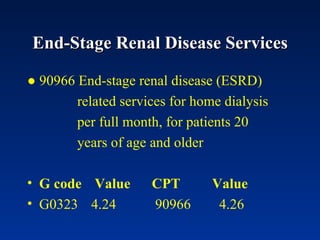
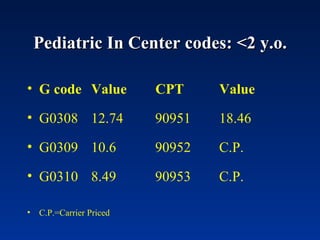
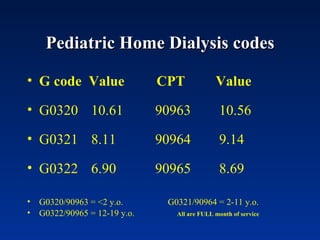
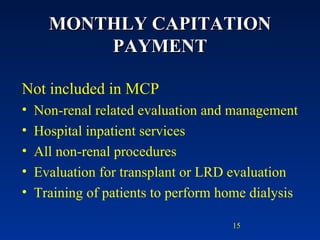
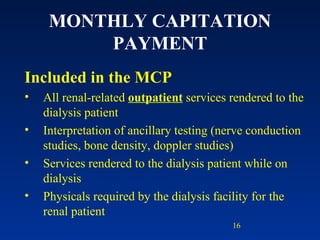
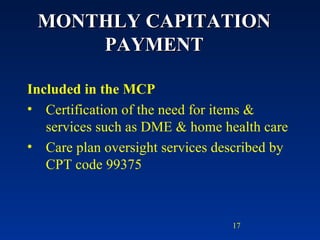
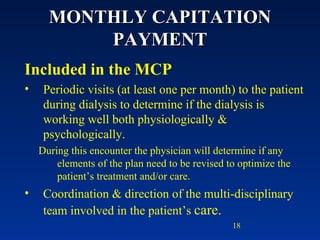
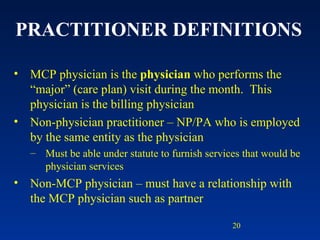
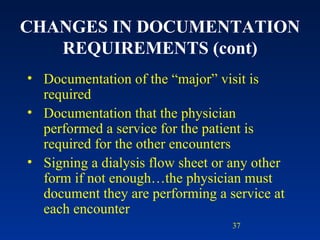
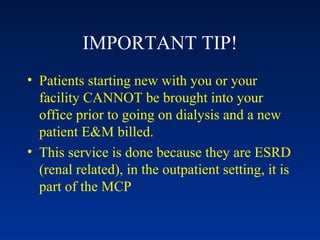
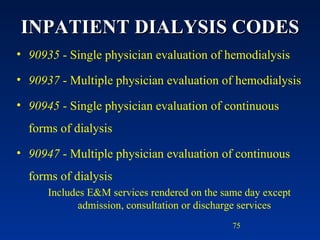
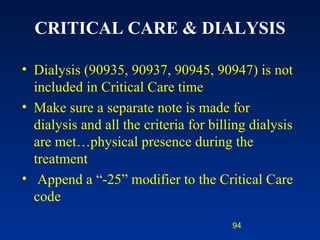
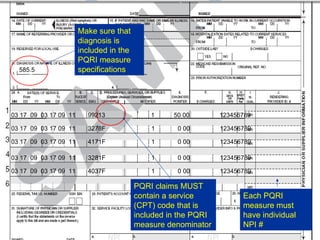
1) New ESRD CPT codes 90951-90970 that replaced previous G and CPT codes, capturing physician work for dialysis patients.
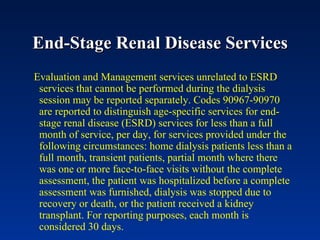
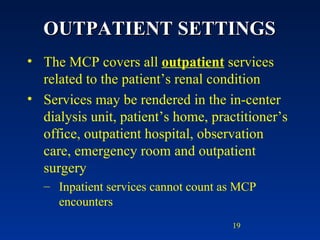
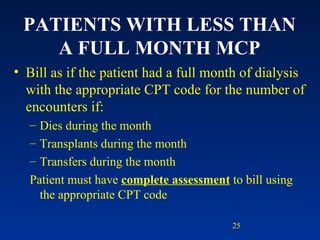
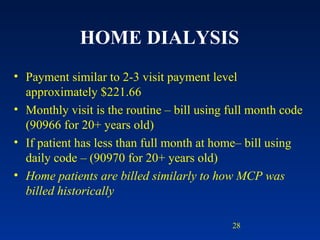
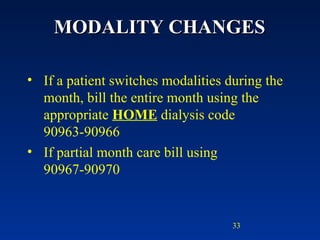
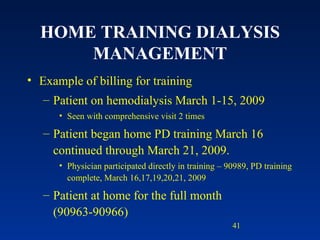
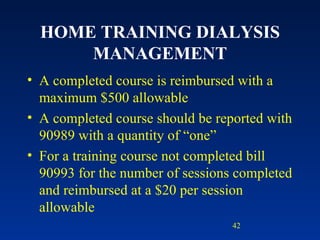
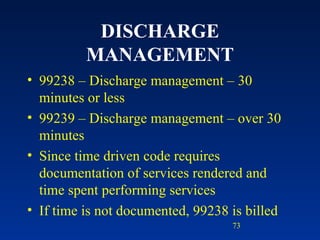
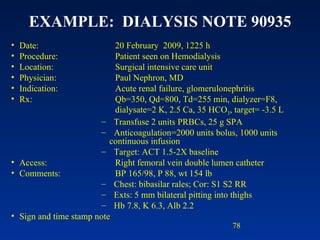
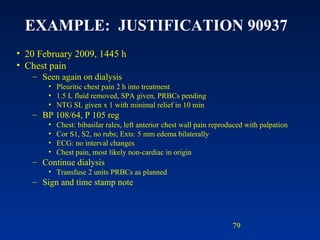
2) Guidelines for billing monthly or daily codes based on full or partial months of service.
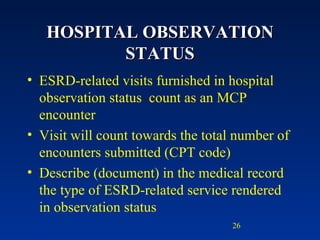
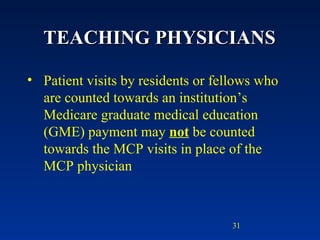
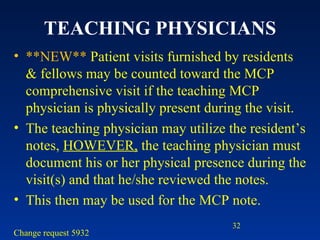
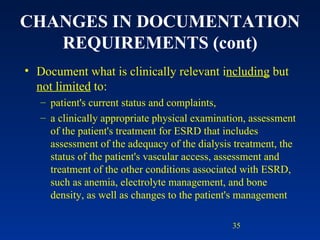
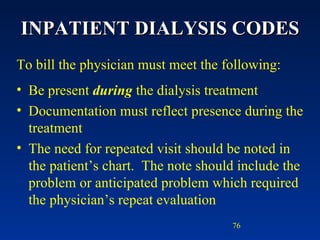
3) Requirements for billing codes accounting for number of face-to-face visits per month.
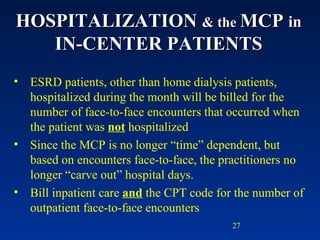
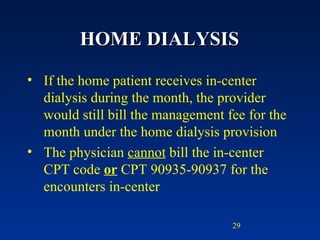
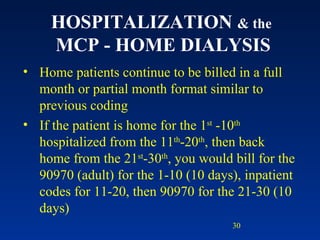
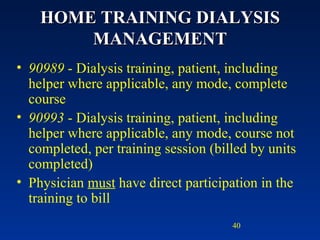
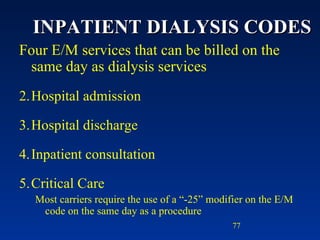
4) Rules around billing for hospitalized, home dialysis, or transient dialysis patients.