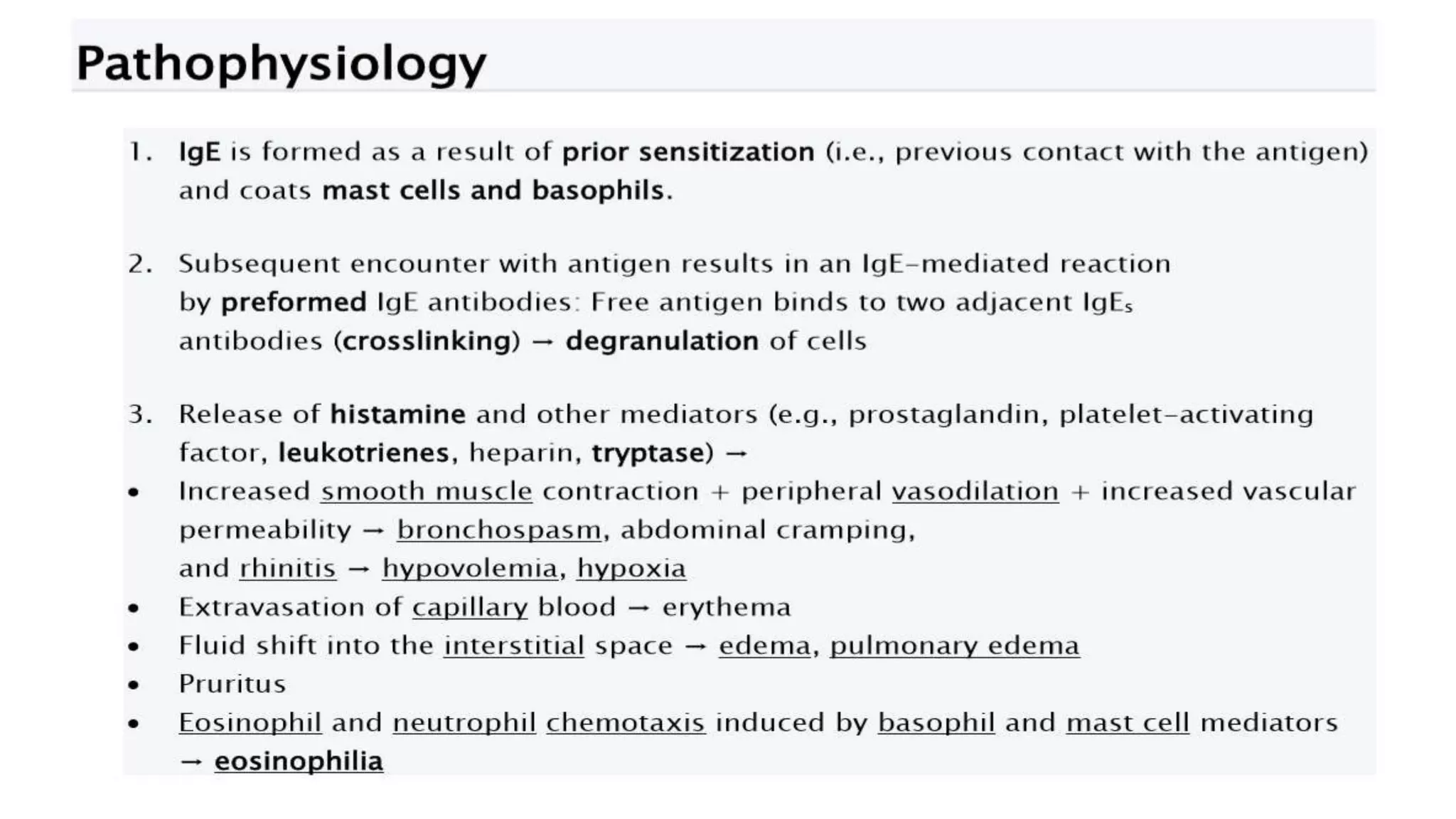
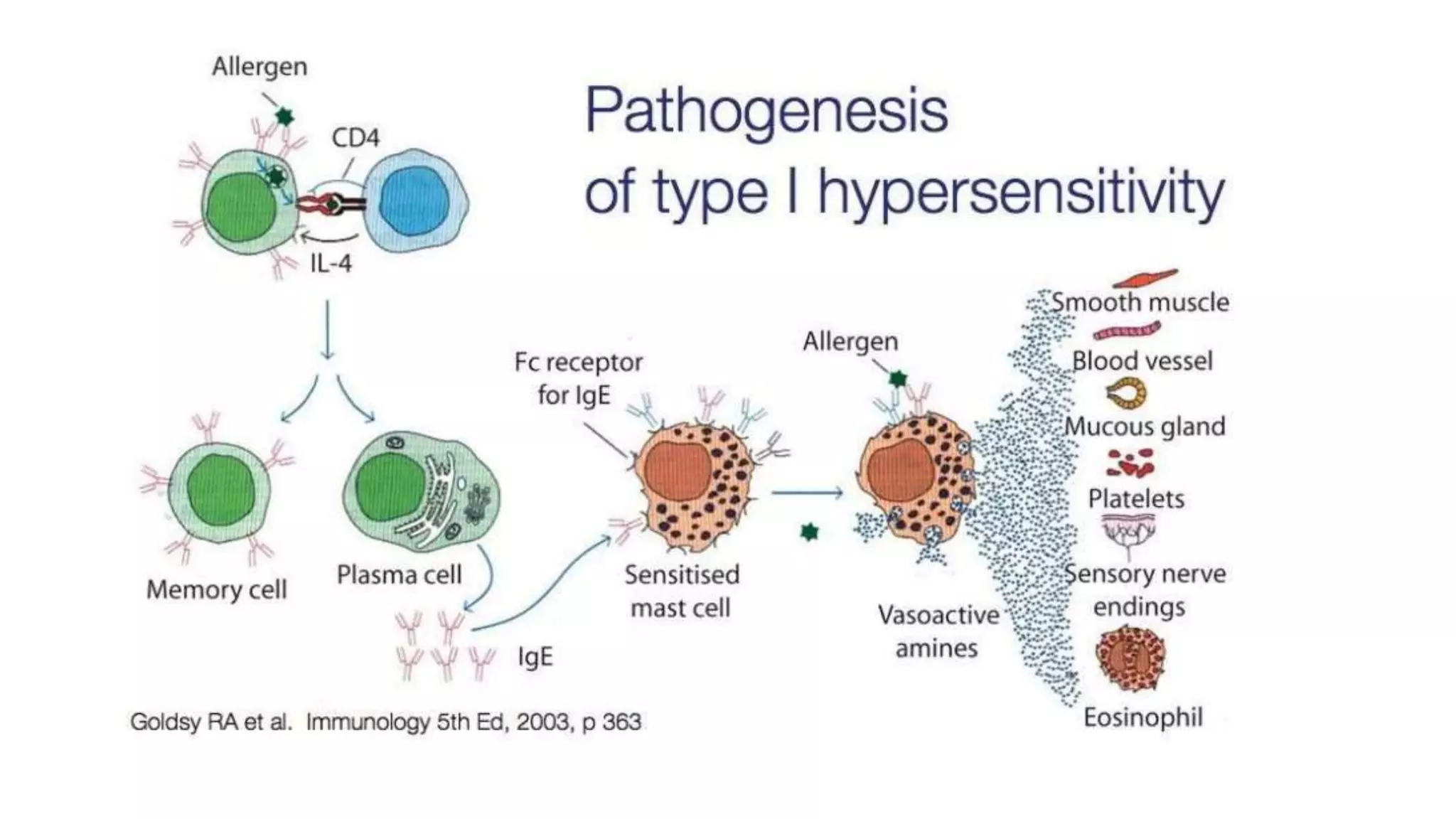
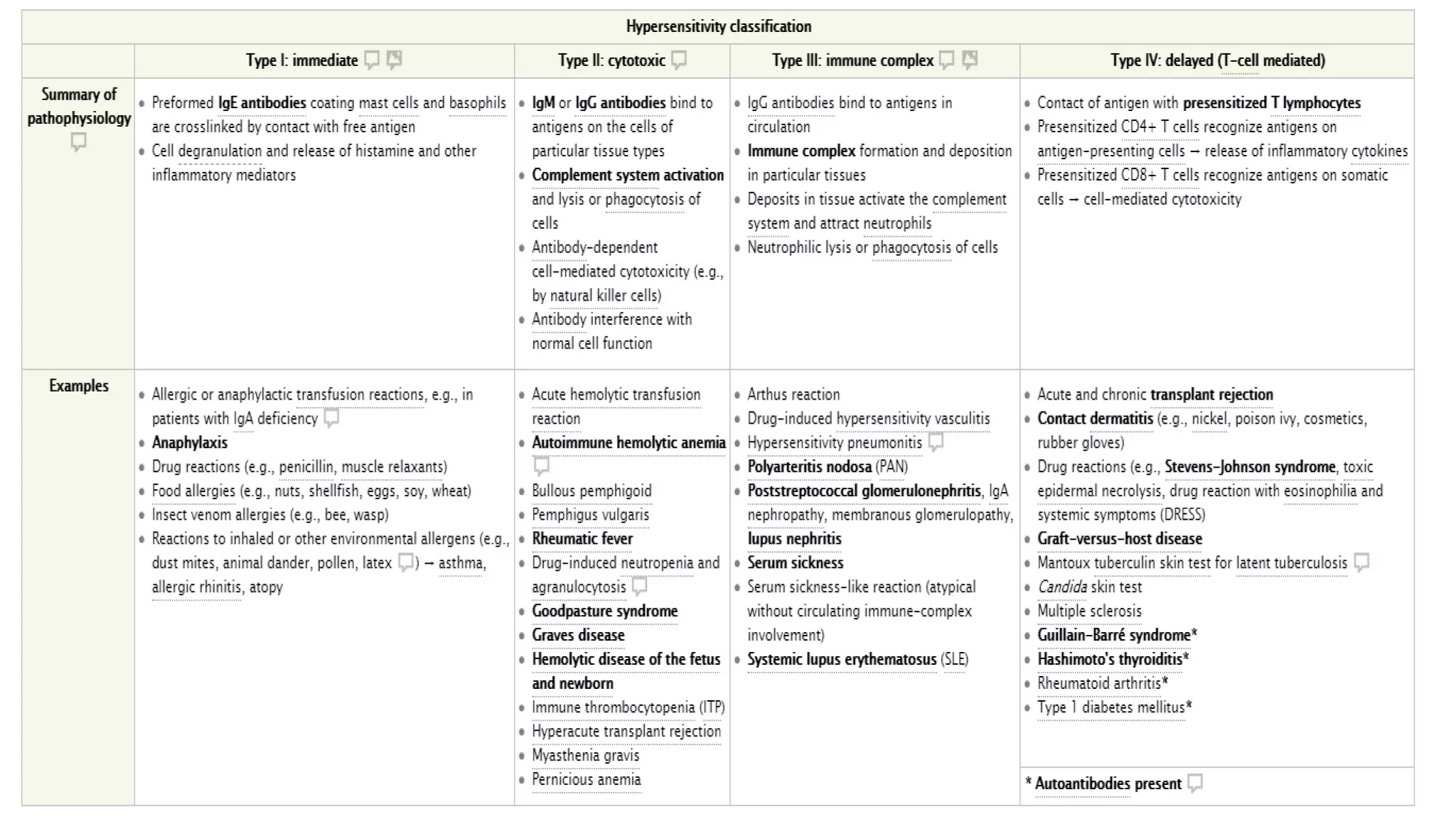
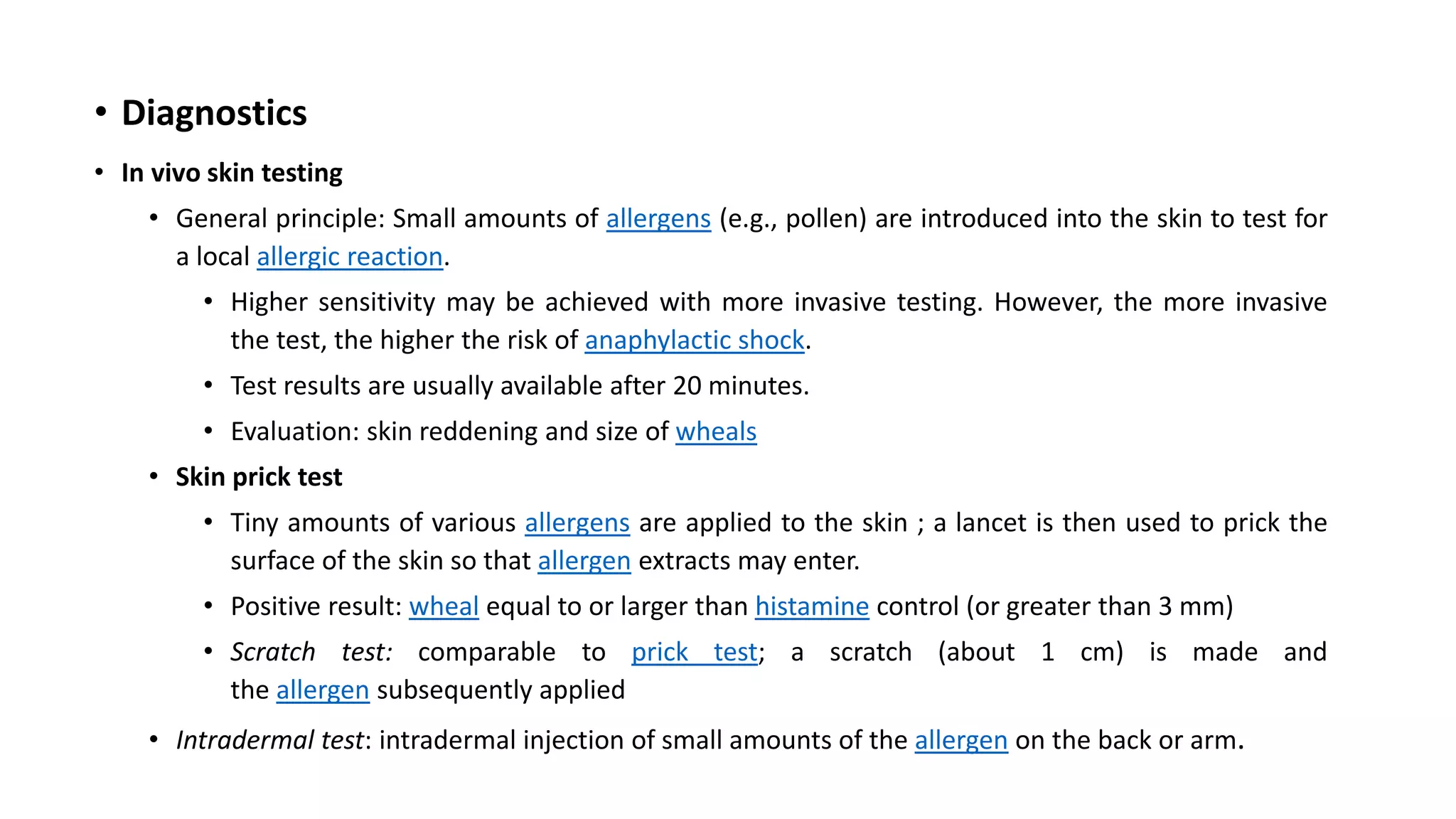
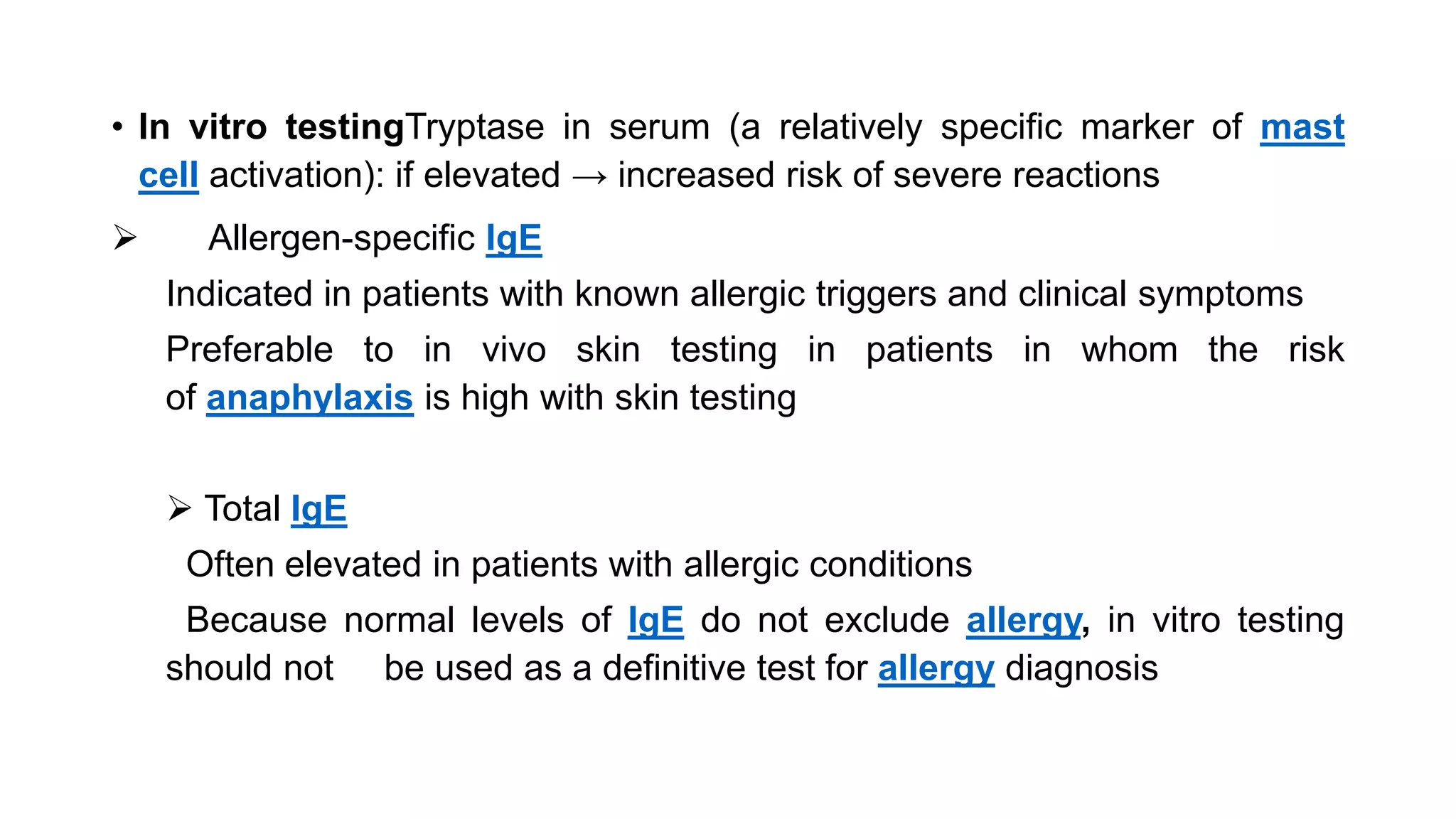
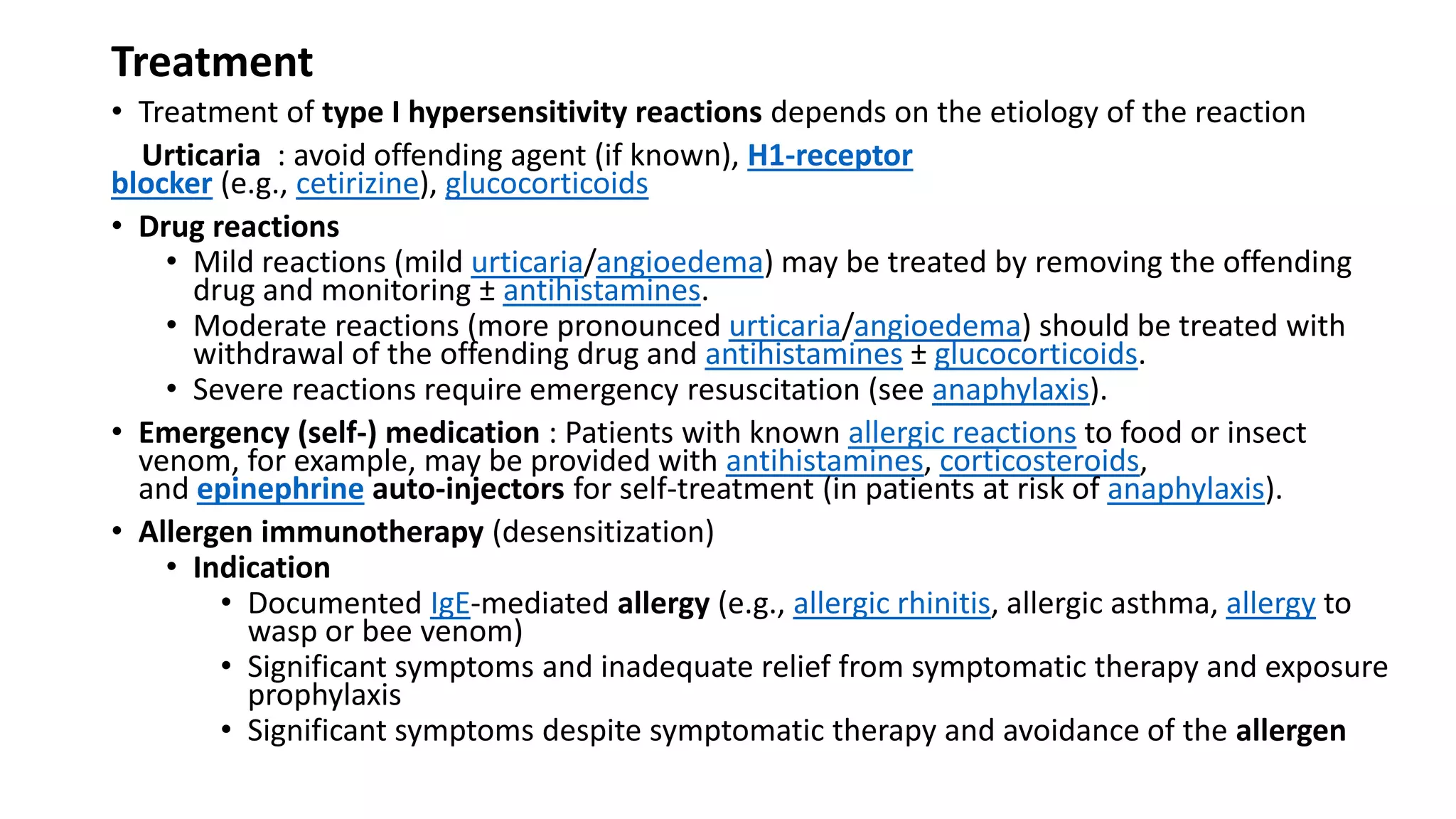
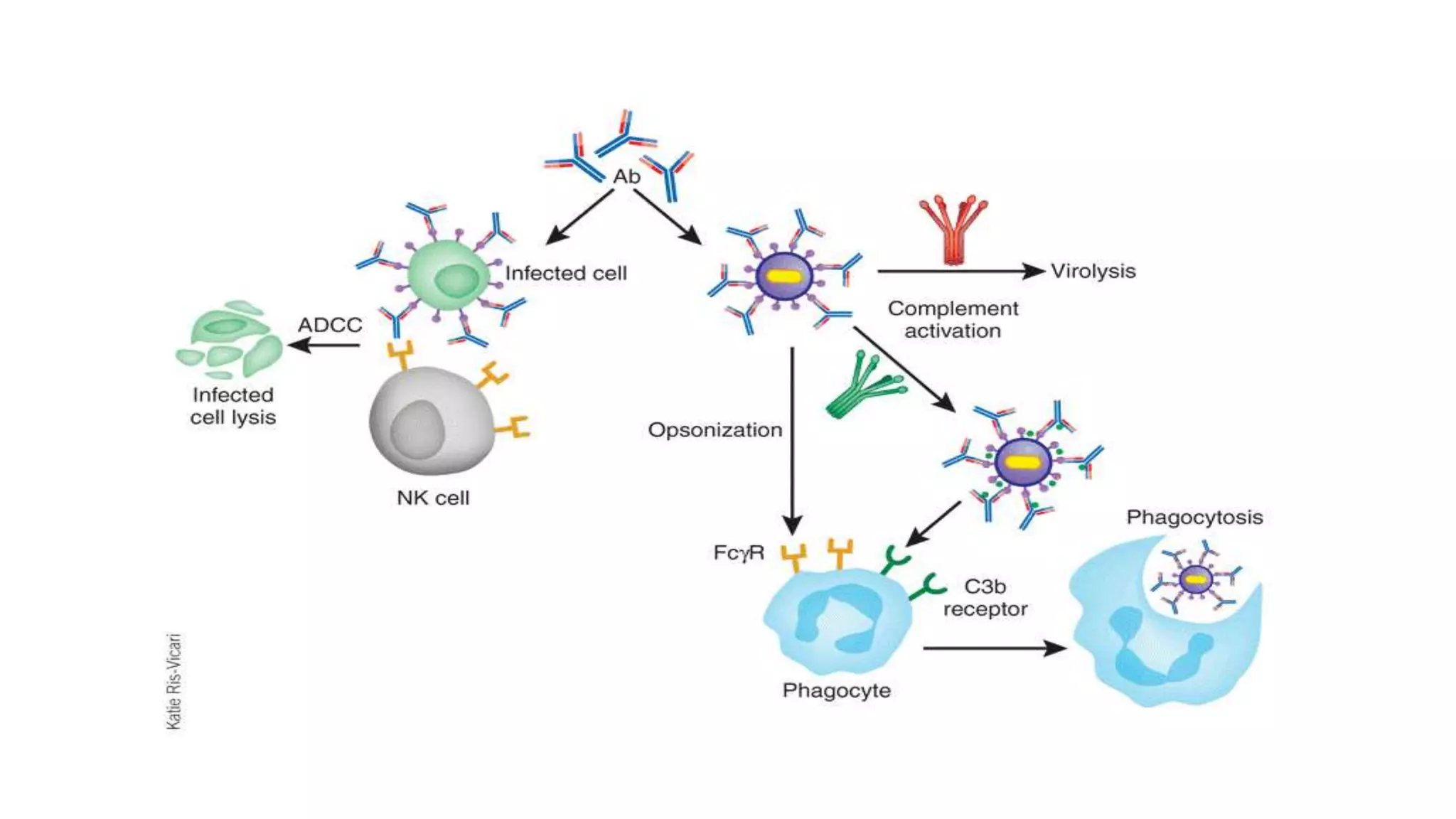
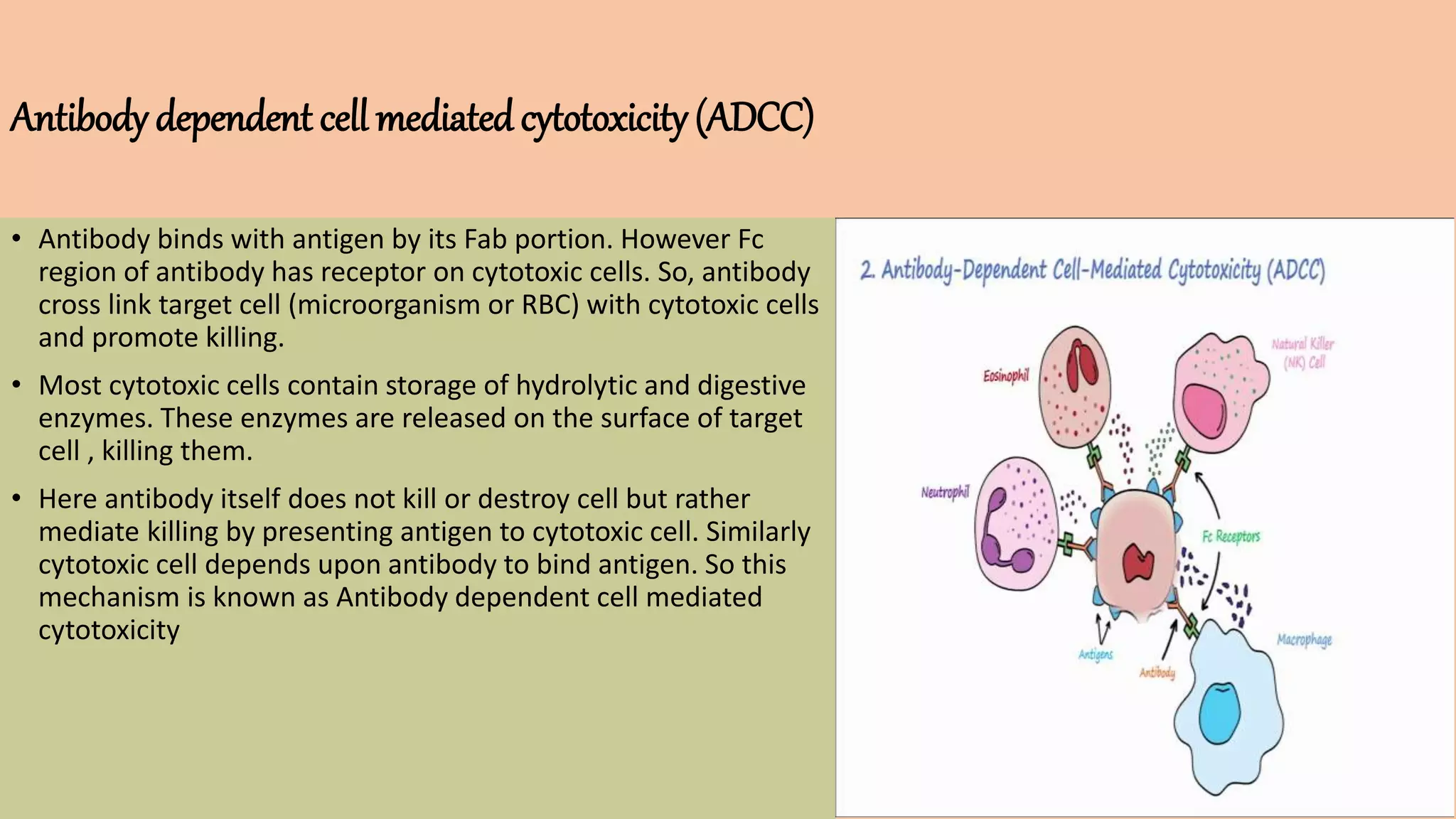
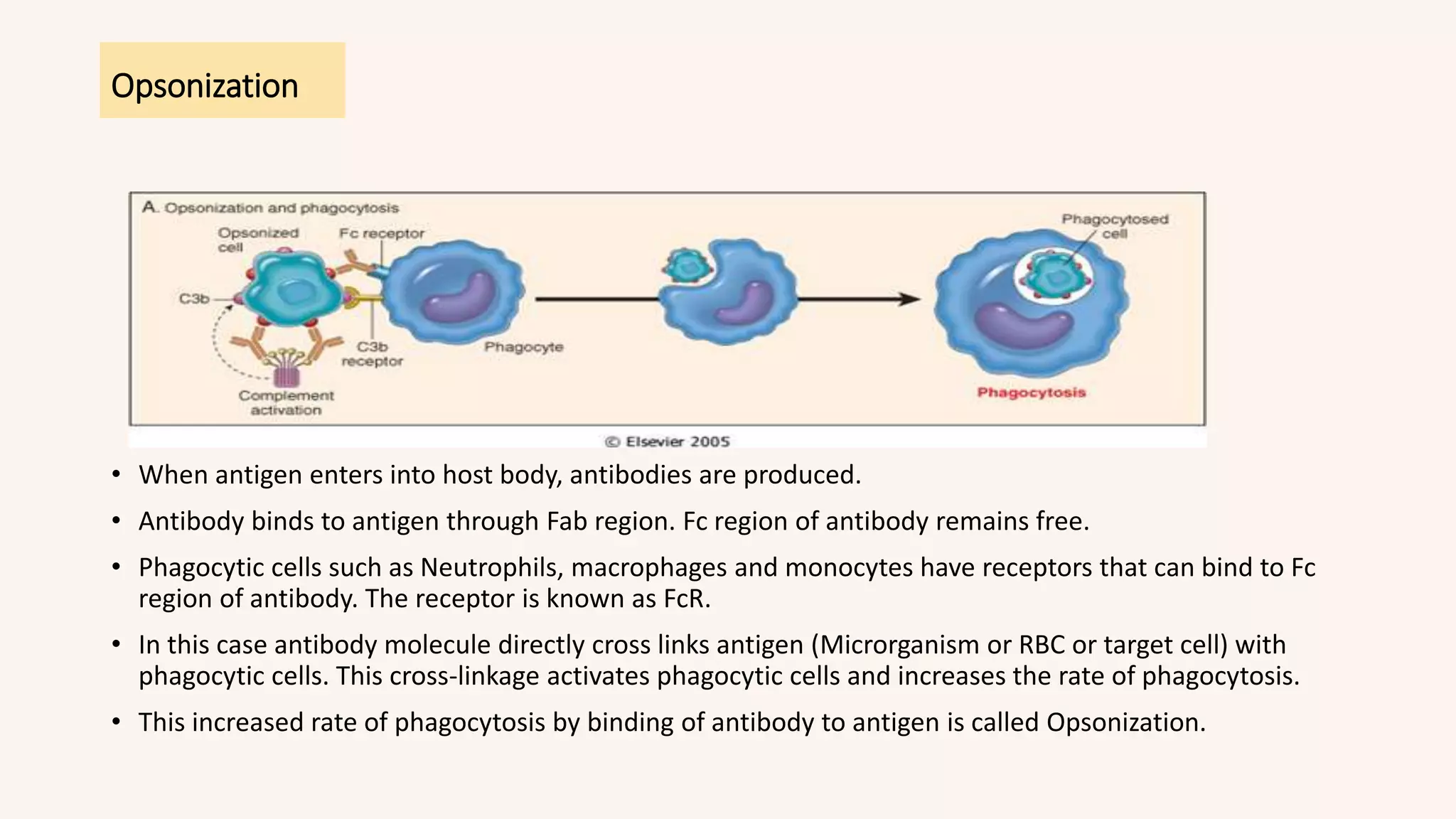
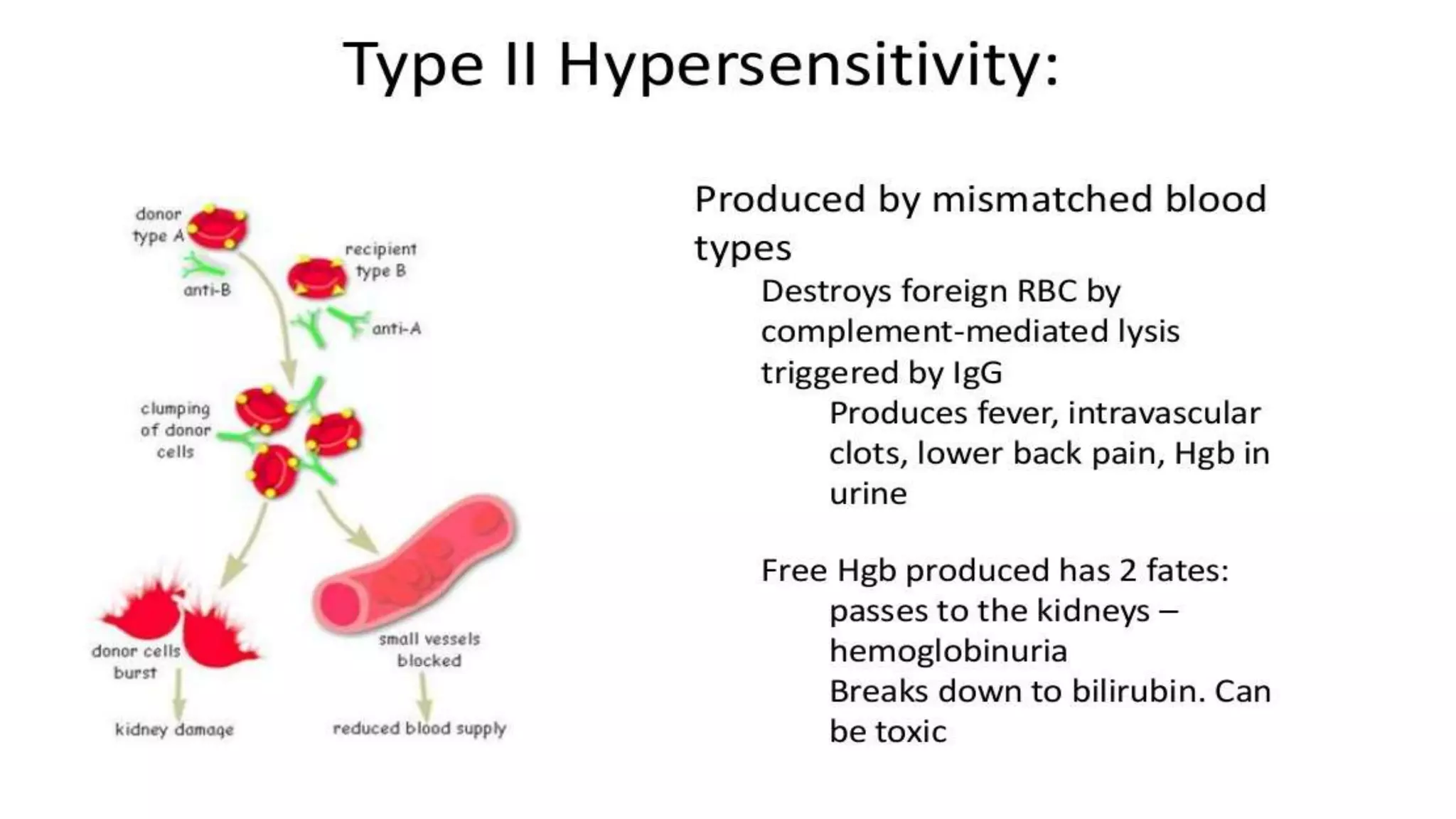
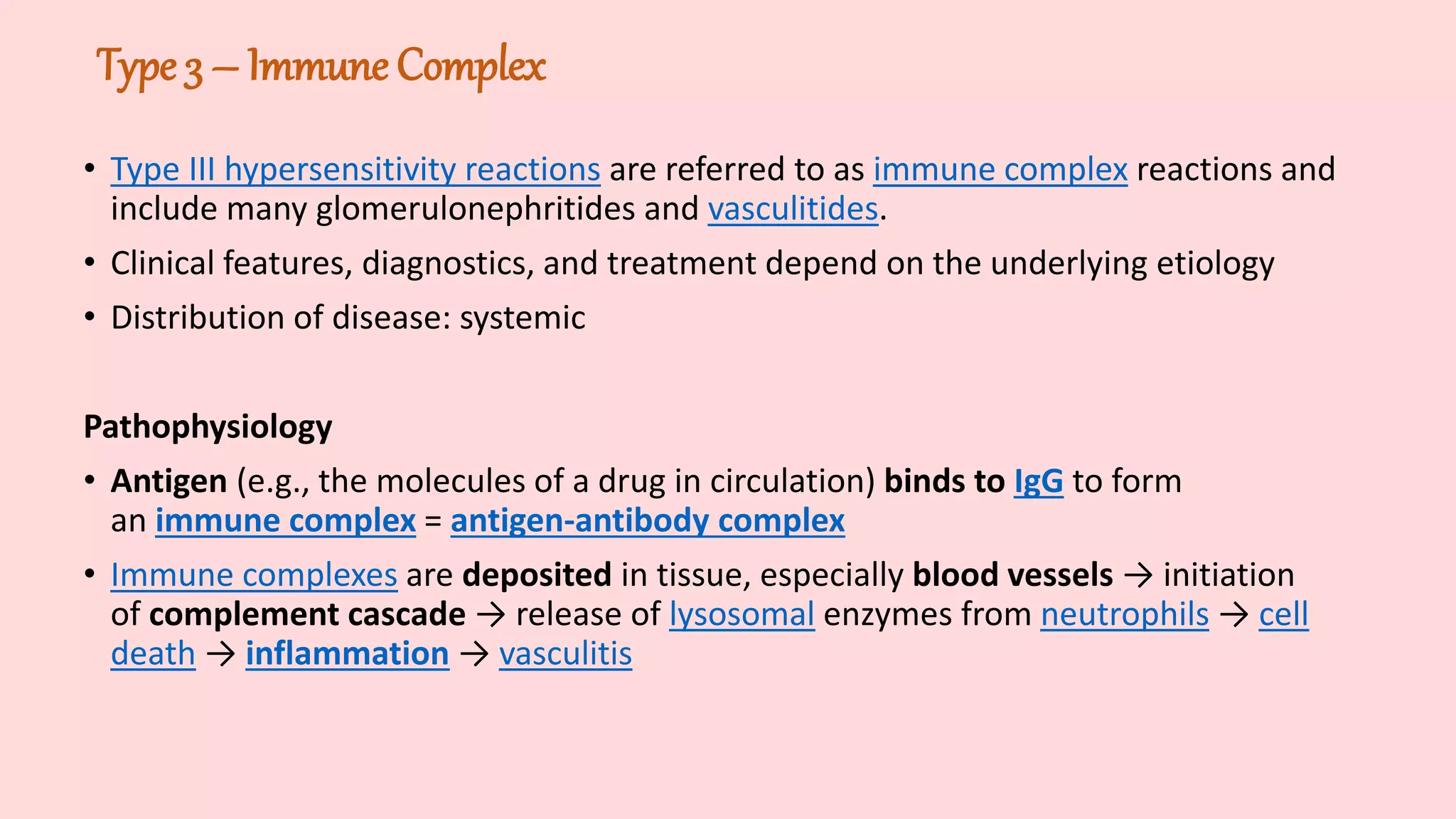
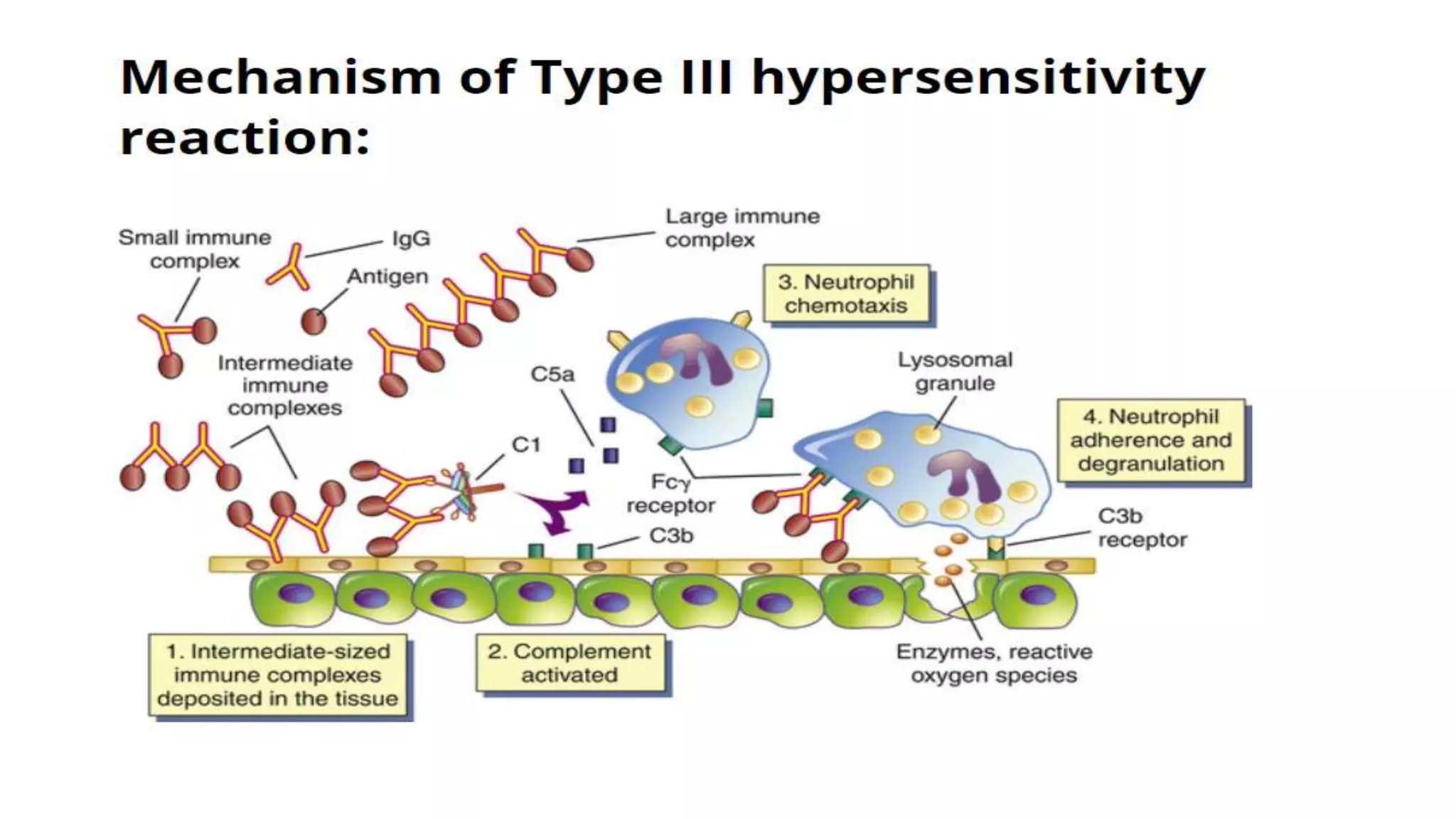
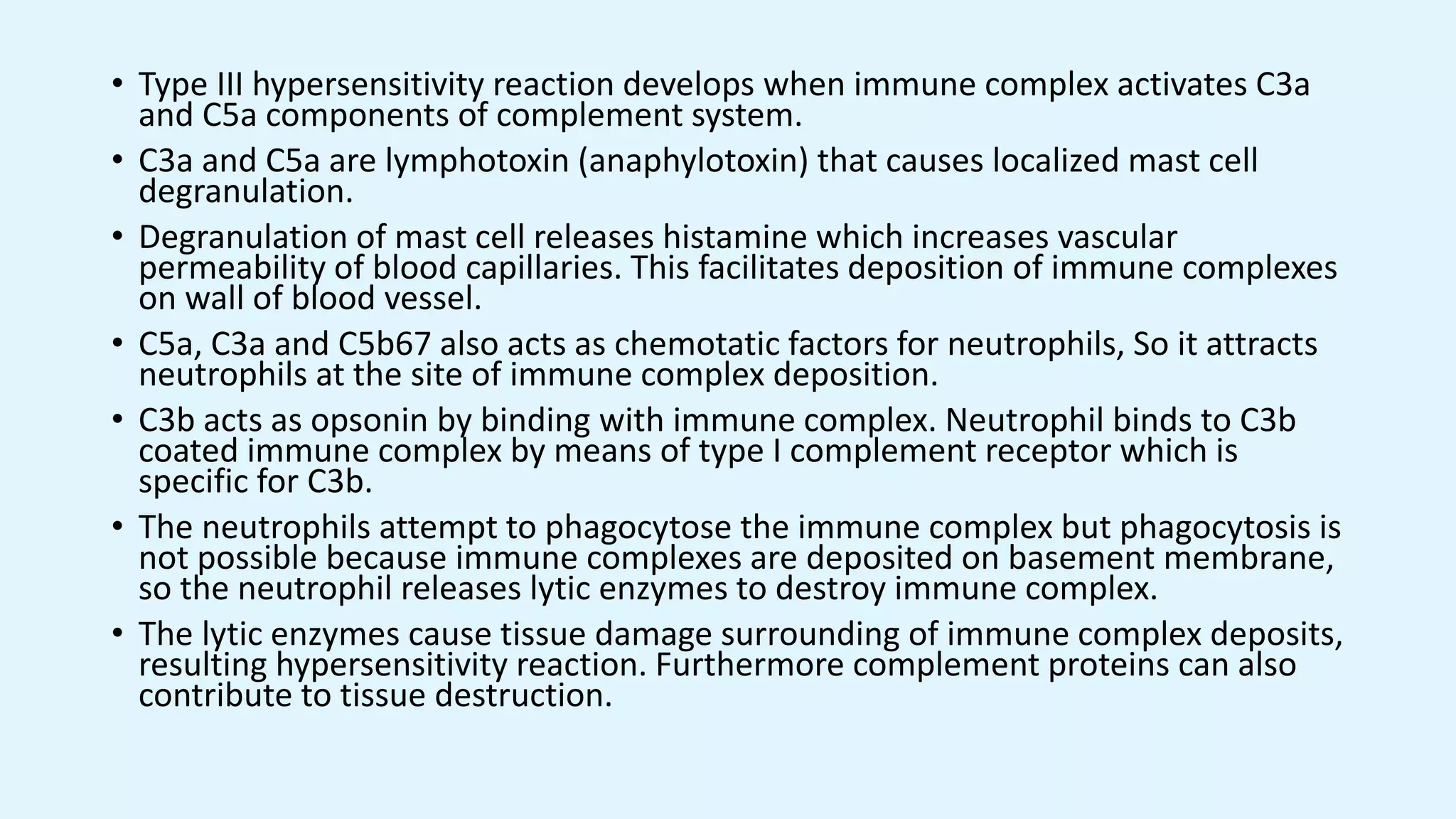
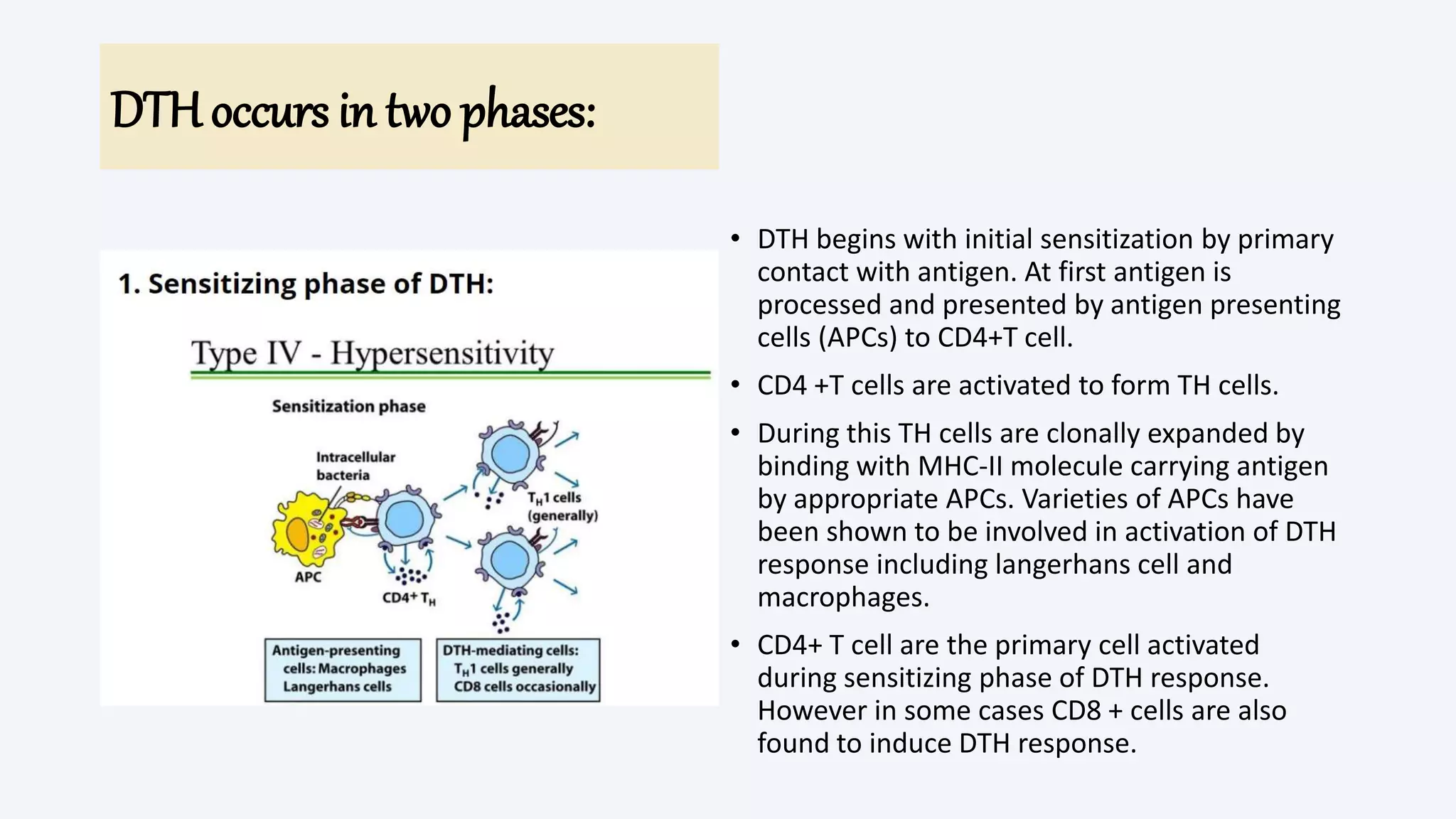
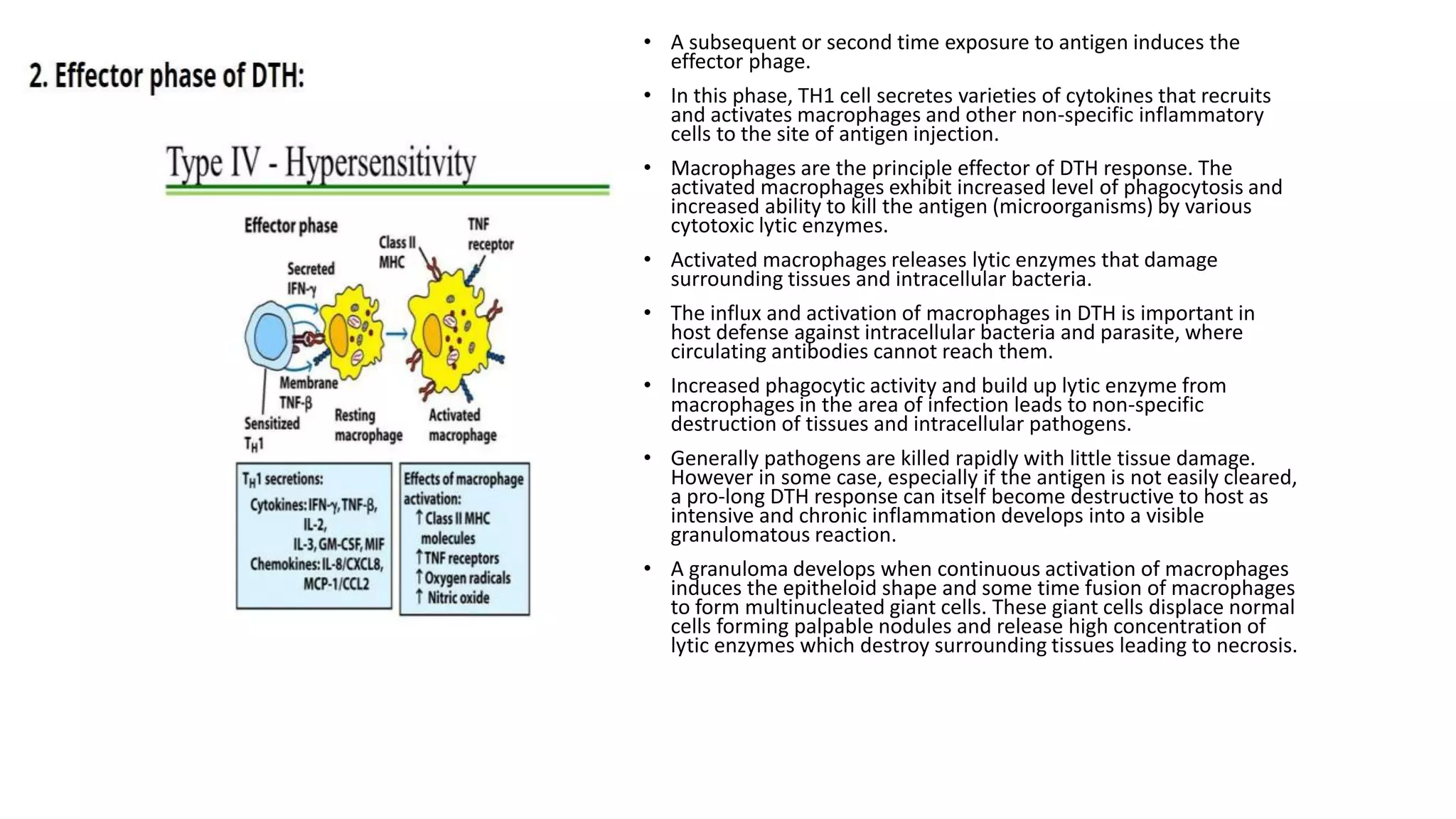
The document discusses hypersensitivity reactions, which are harmful immune responses to typically harmless antigens, classifying them into four types: Type I (immediate), Type II (cytotoxic), Type III (immune complex), and Type IV (cell-mediated). Each type has distinct clinical features, diagnostic methods, and treatment approaches, with Type I offering symptoms like anaphylaxis and requiring fast intervention, while Type IV involves delayed reactions primarily mediated by T cells. The text outlines associated conditions, testing methods, and treatment strategies for various allergic and autoimmune reactions.