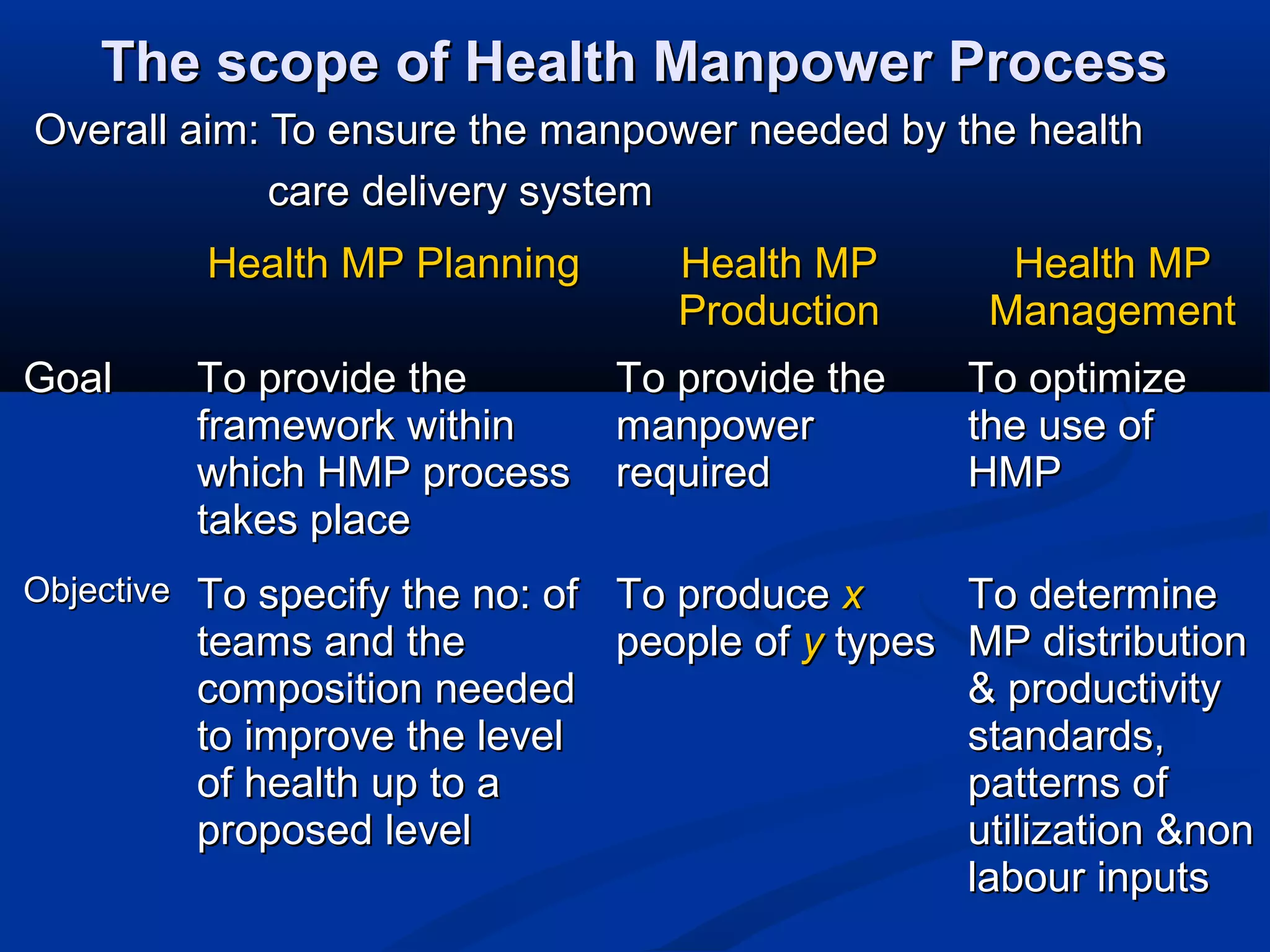
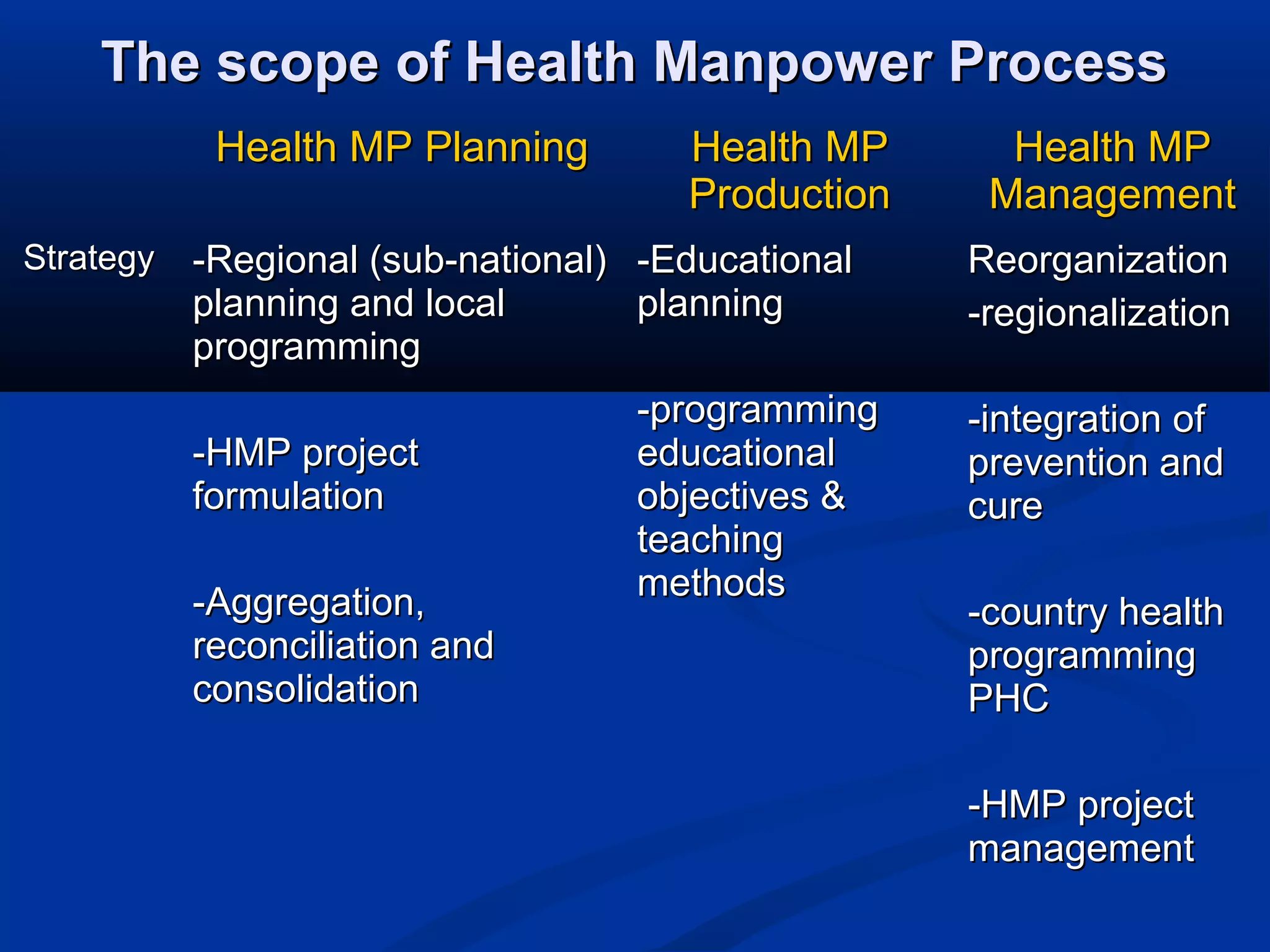
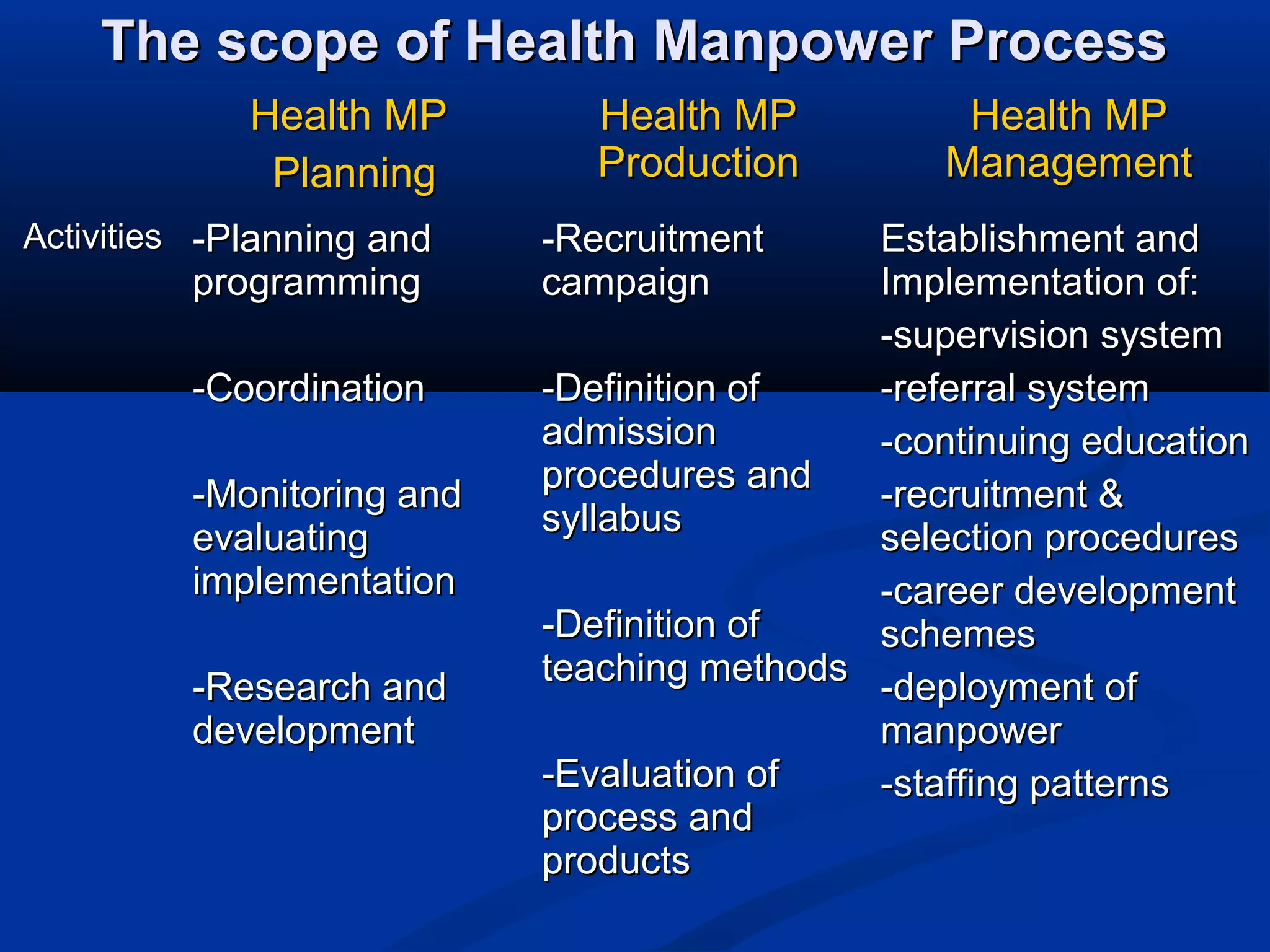
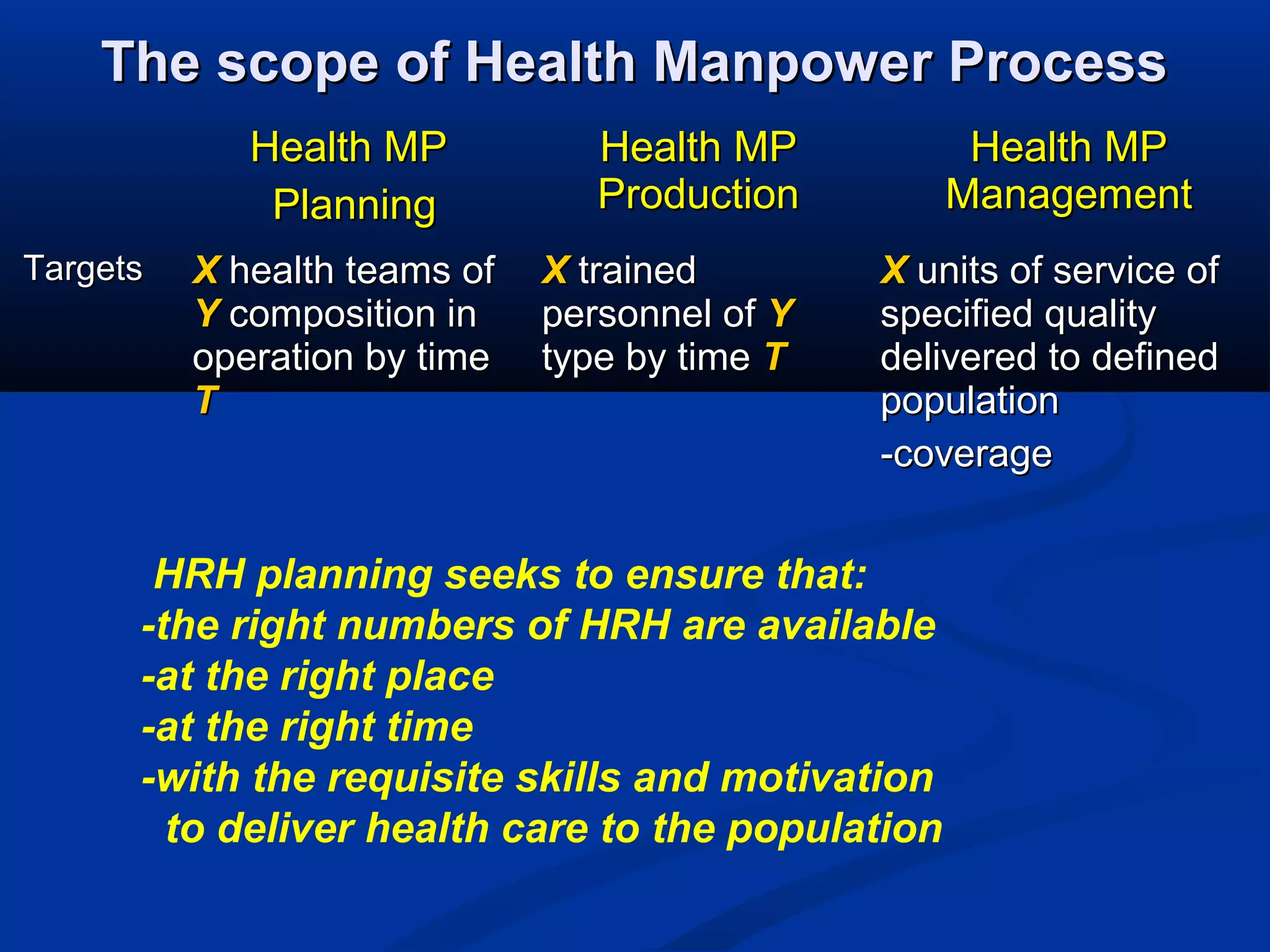
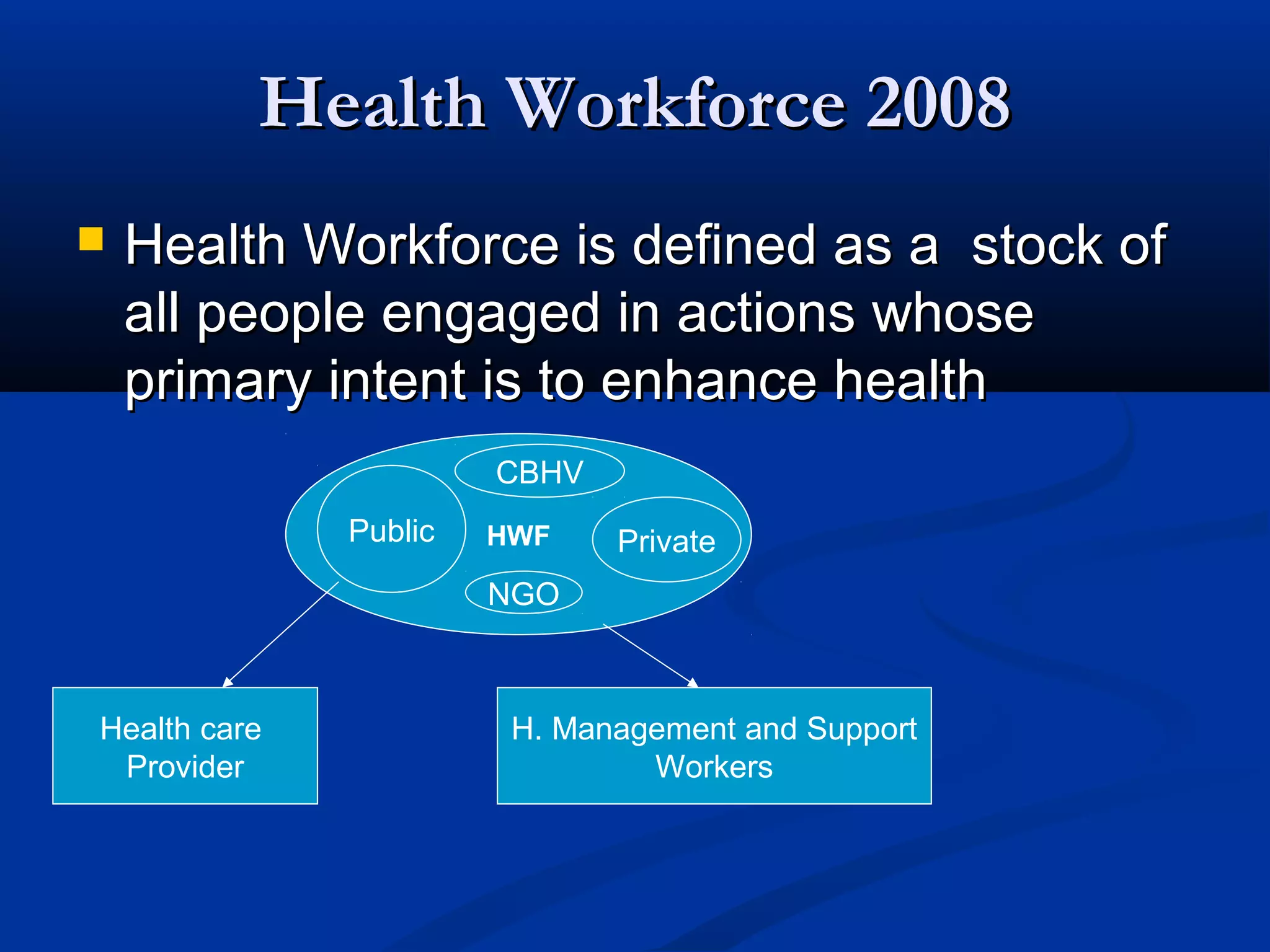
The document discusses several issues related to health workforce planning, production, and management in developing countries. Some key points include:
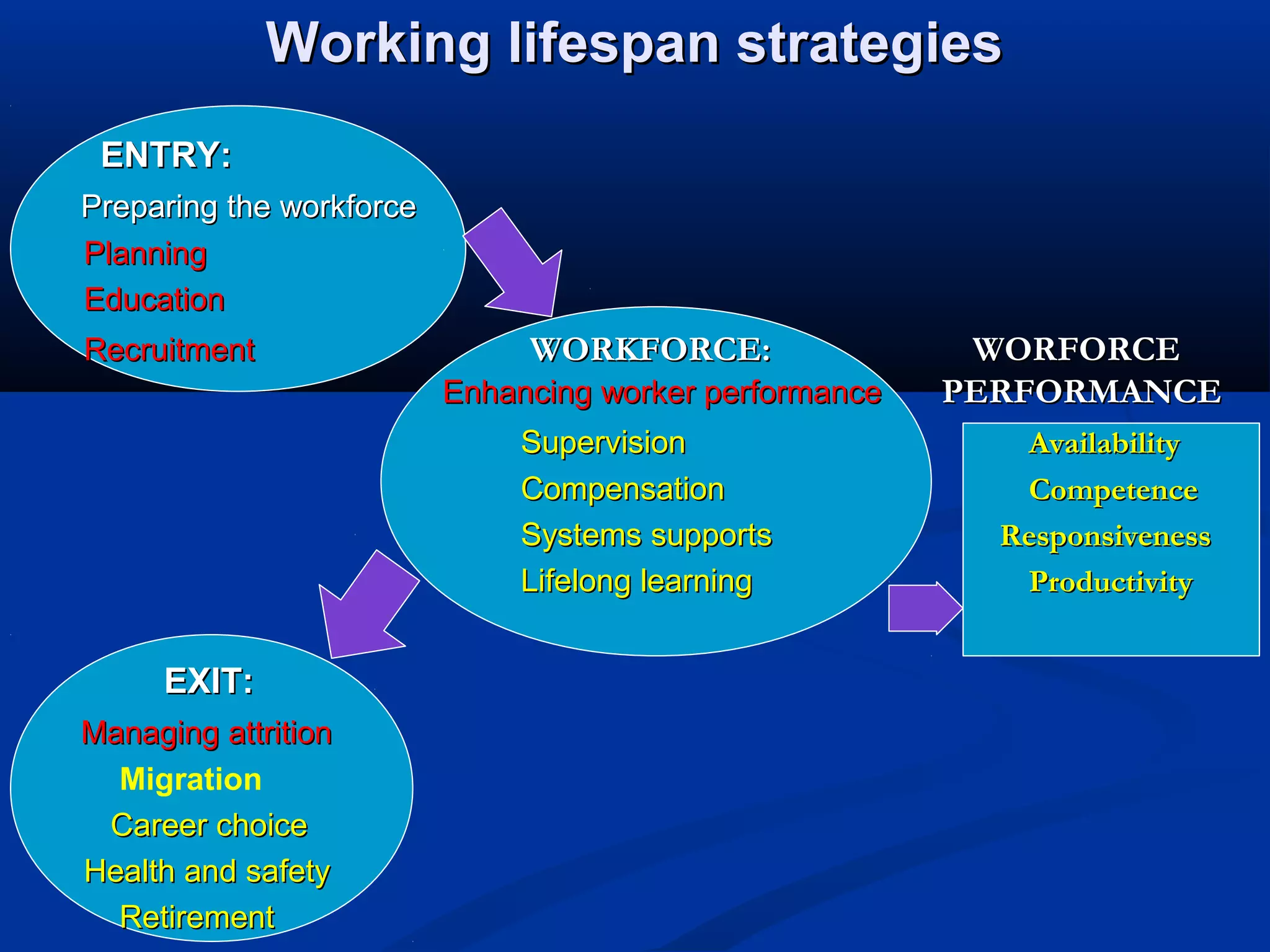
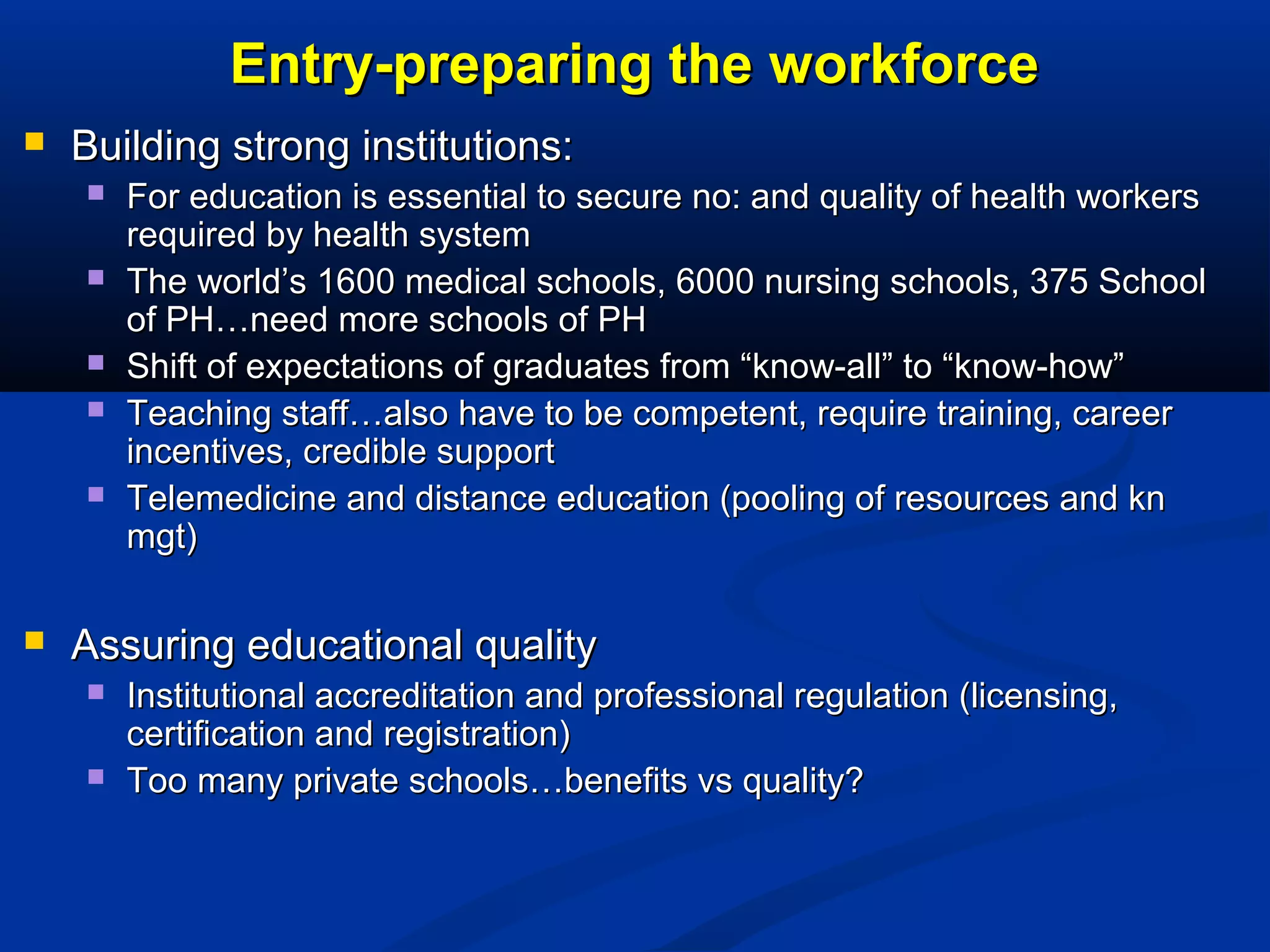
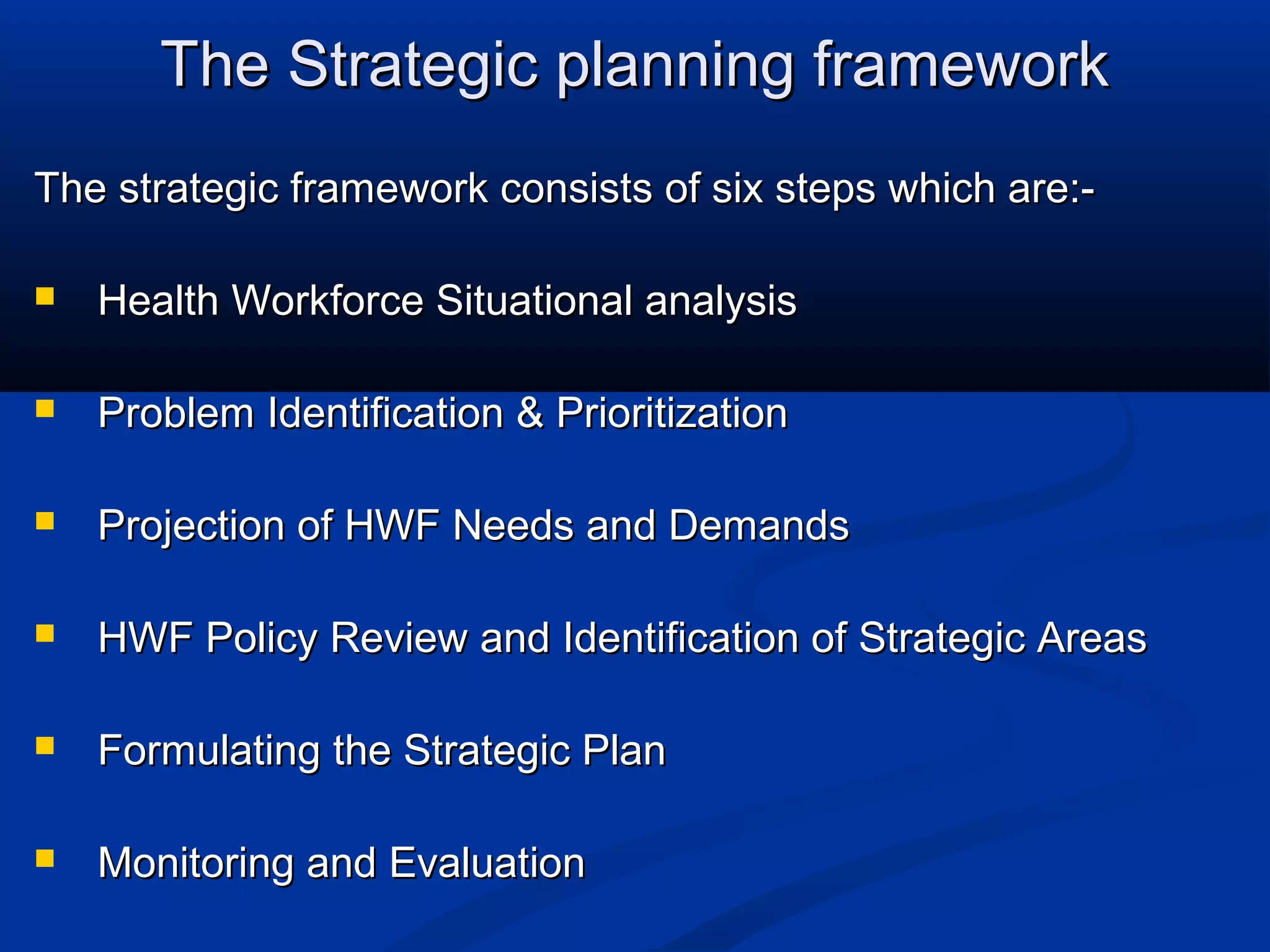
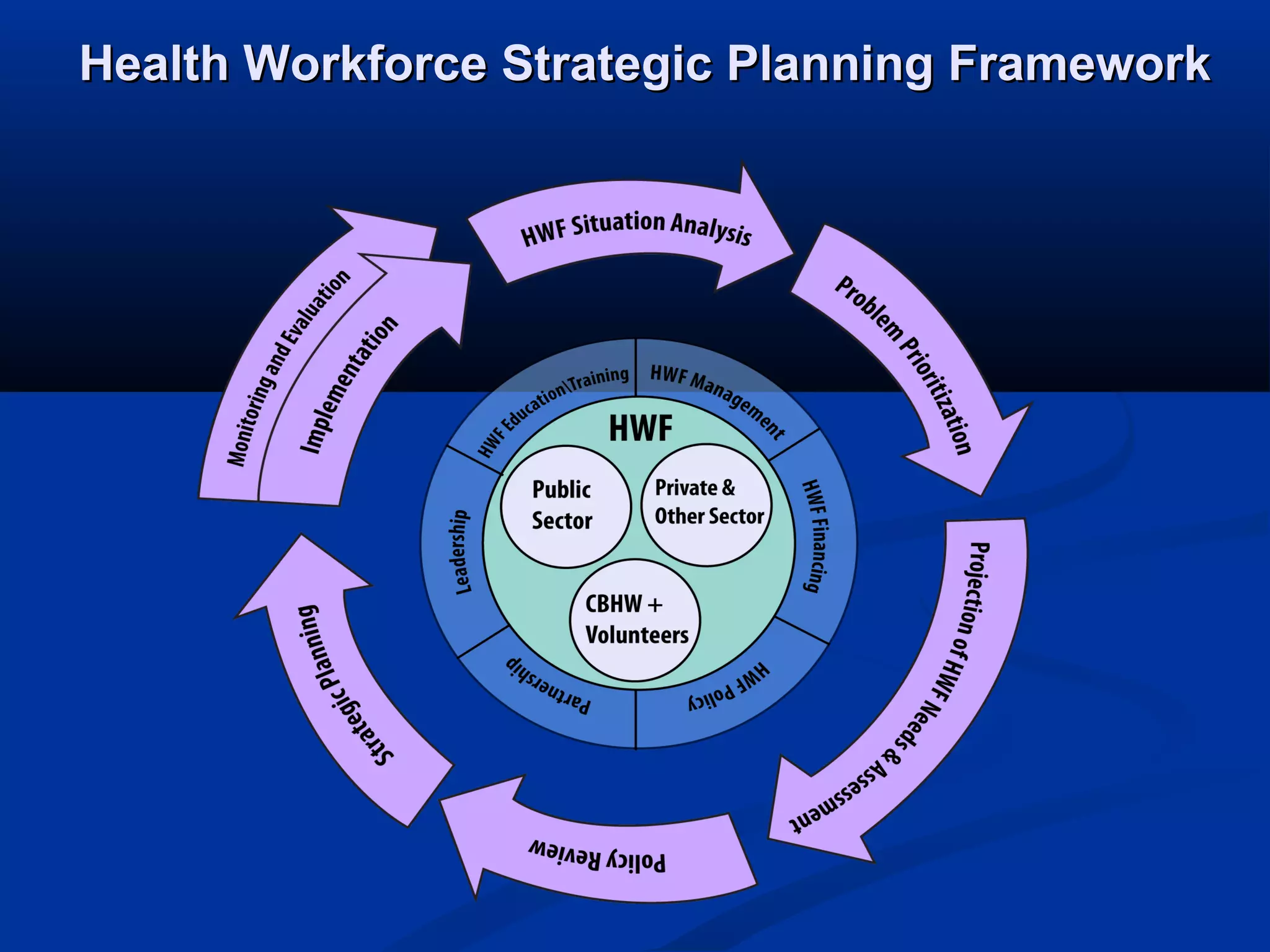
1) Health workforce planning seeks to ensure the appropriate number, distribution, skills, and motivation of health workers to deliver healthcare.
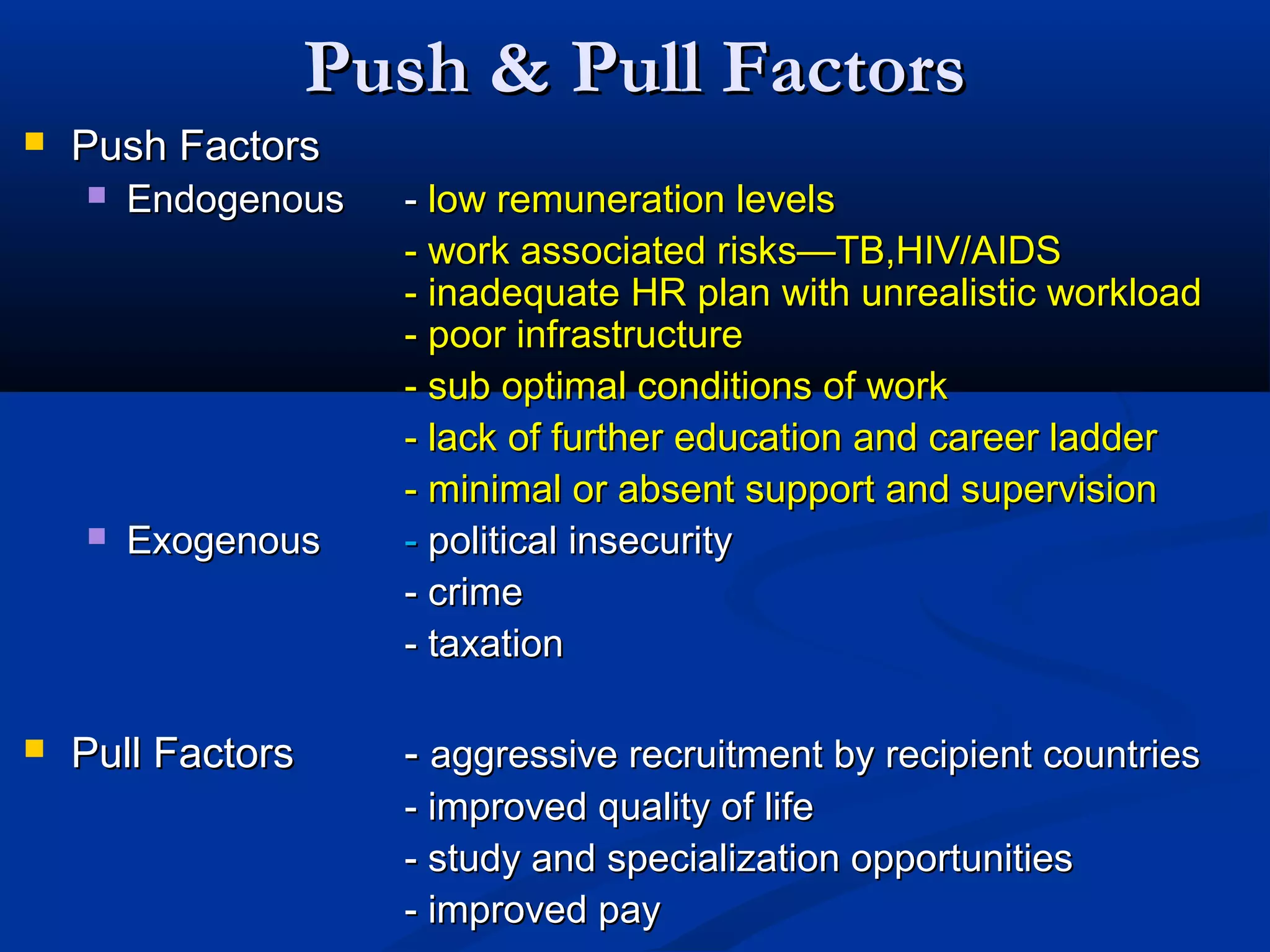
2) Issues like mismatched training and jobs, lack of rural positions, and emigration of physicians hamper effective health workforce management.
3) Factors like education, management, financing, policy, partnerships, and leadership influence a country's ability to develop, sustain, and optimize its health workforce.