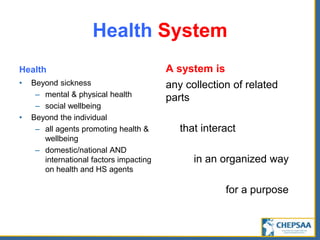
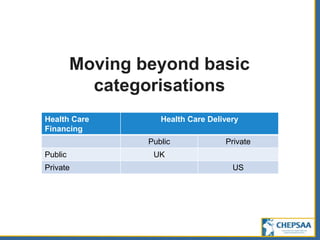
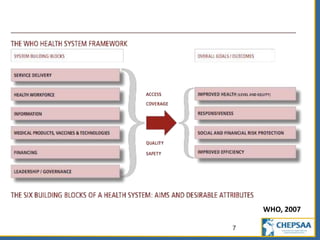
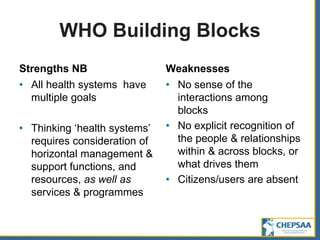
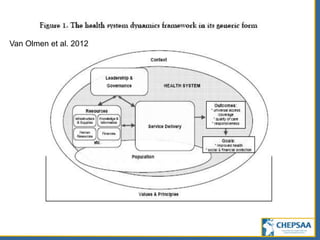
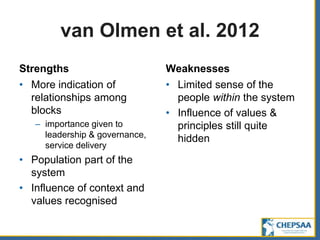
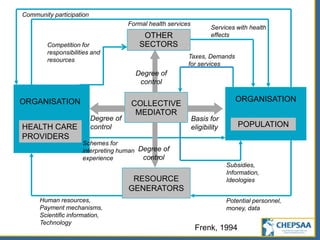
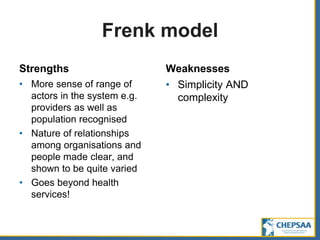
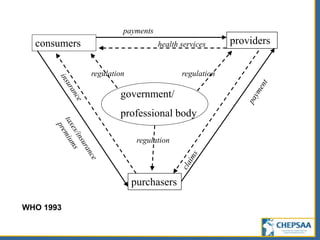
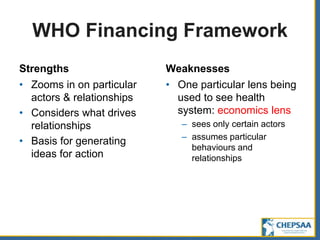
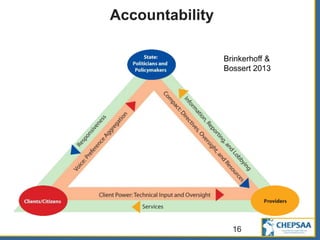
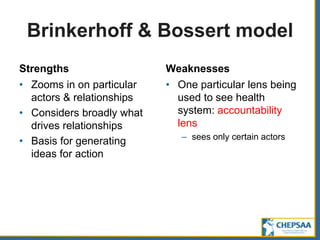
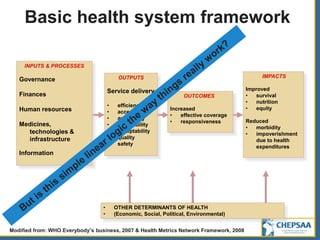
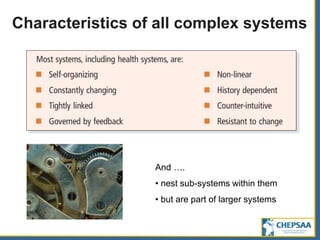
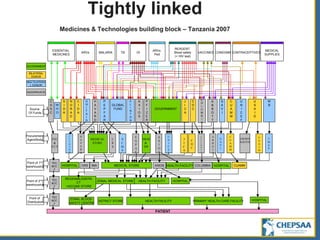
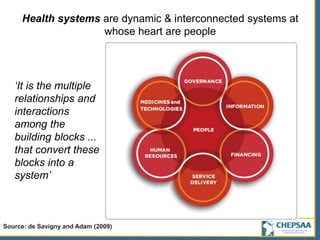
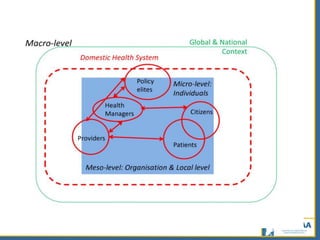
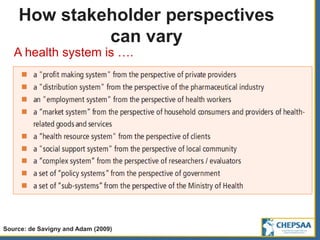
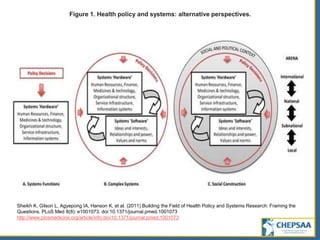
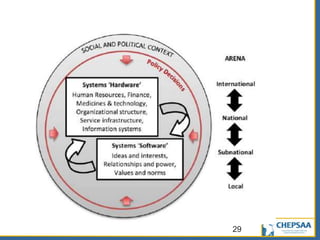
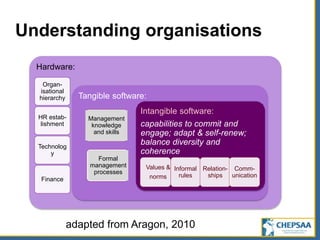
This document provides an overview of conceptual frameworks for understanding health systems. It defines a health system as all organizations, people and actions whose primary intent is to promote, restore or maintain health. It discusses several frameworks developed by the WHO and others to conceptualize the different components, actors and relationships within health systems. It acknowledges that health systems are complex and dynamic, with unpredictable paths of implementation for interventions. The document emphasizes that health systems should be viewed holistically as interconnected systems centered around people.