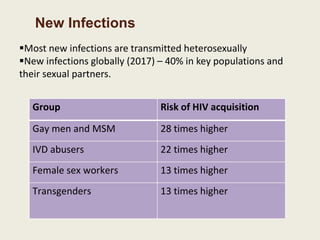
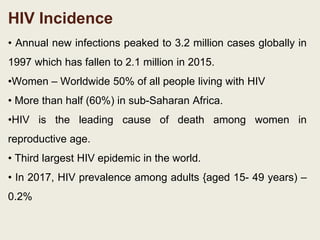
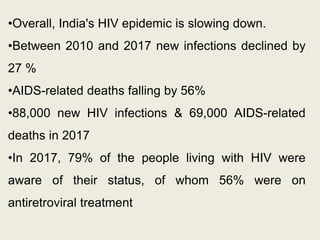
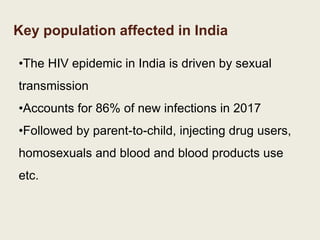
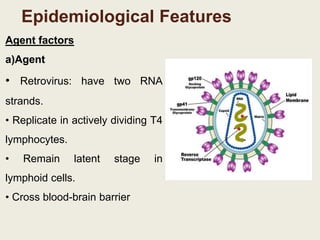
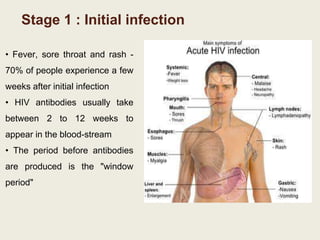
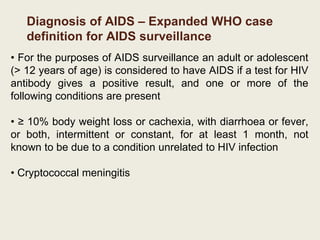
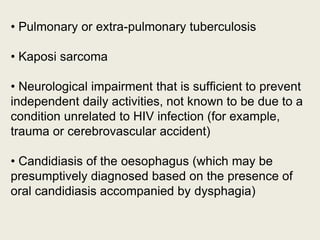
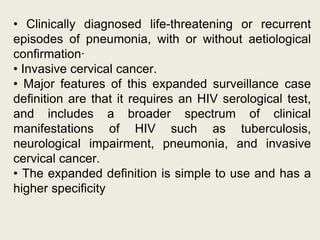
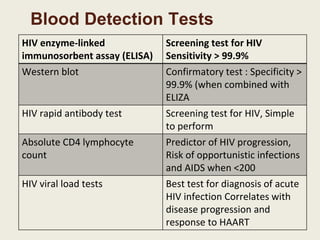
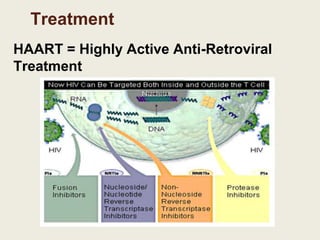
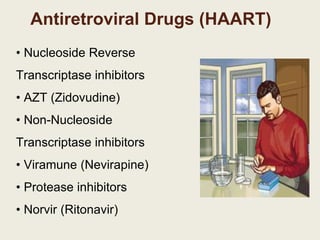
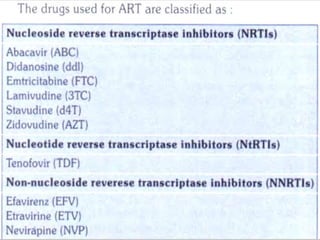
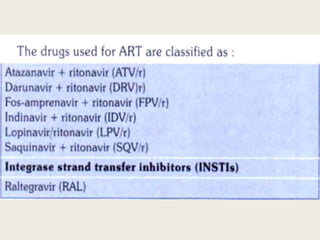
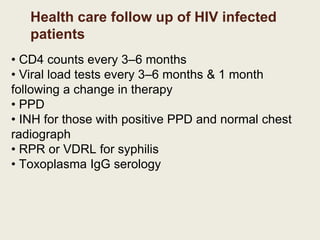
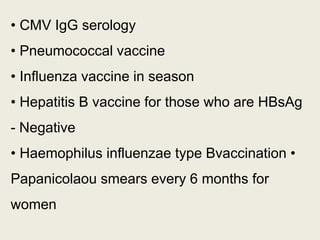
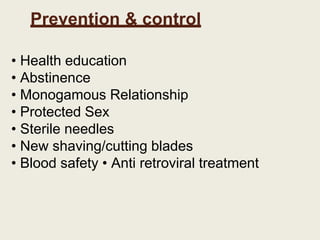
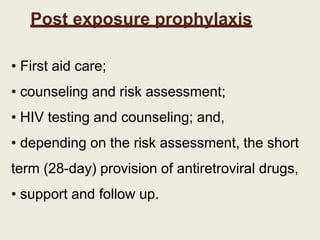
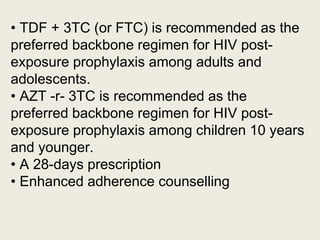
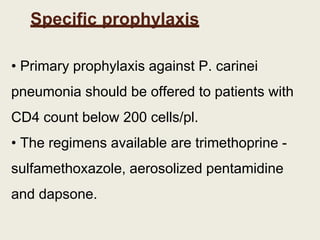
HIV/AIDS is caused by the HIV virus and weakens the immune system. It is transmitted through unprotected sex, blood contact, mother-to-child transmission and intravenous drug use. India's epidemic is slowing but certain groups like sex workers, truck drivers and migrant workers remain at high risk. Diagnosis involves antibody tests and monitoring CD4 counts and viral load. Treatment is lifelong antiretroviral therapy. Prevention focuses on education, condoms, sterile needles and post-exposure prophylaxis.