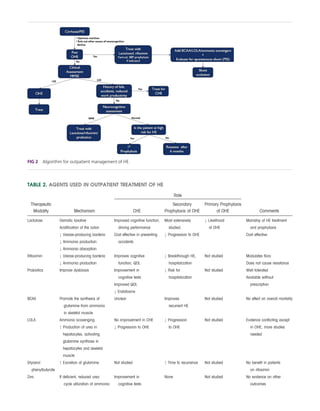
Hepatic encephalopathy (HE) refers to brain dysfunction caused by liver disease and can range from subclinical to coma. Minimal HE (MHE) and grade I HE are now classified as covert HE (CHE) due to difficulty distinguishing without tests. CHE affects 40-84% of cirrhotics and is associated with reduced quality of life, impaired skills, and survival. Treatment of CHE is justified given these consequences. Lactulose, rifaximin, probiotics, and diet modifications can improve CHE symptoms. Specialized tests are needed to diagnose MHE, while CHE screening tools like SIP-CHE can provide rapid assessment.