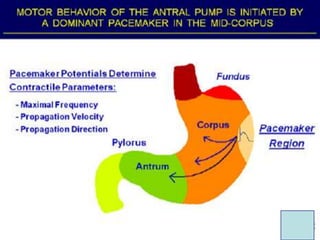
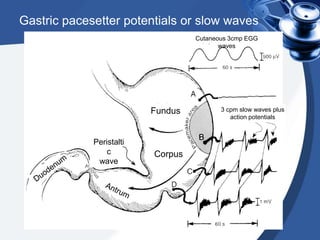
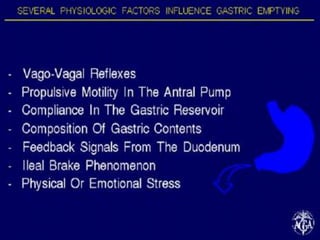
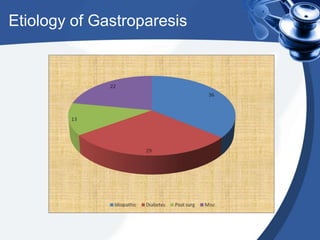
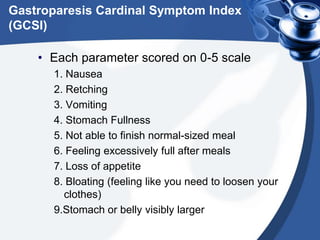
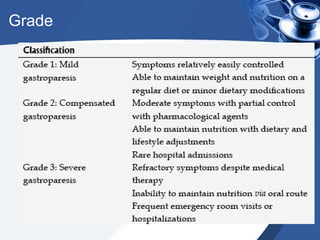
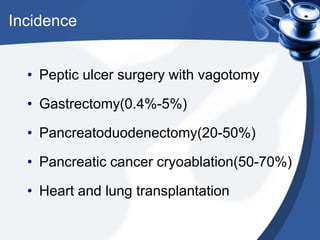
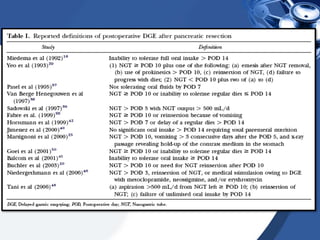
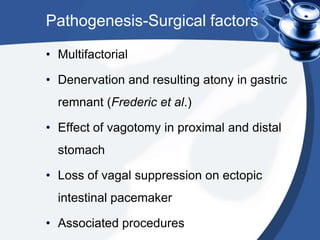
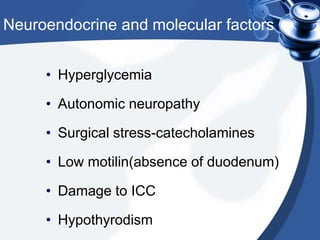
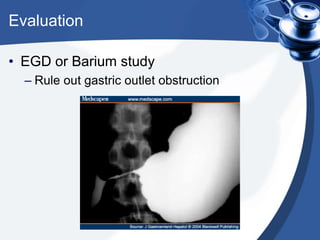
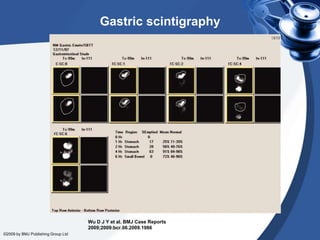
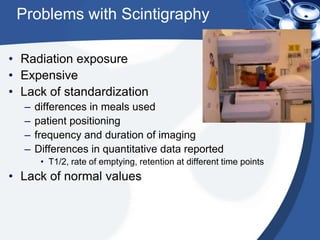
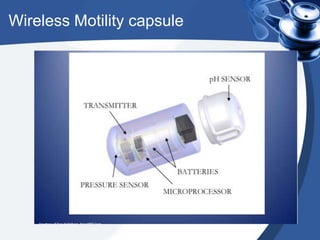
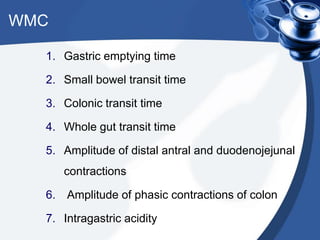
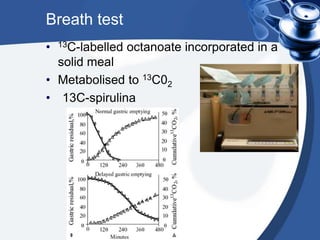
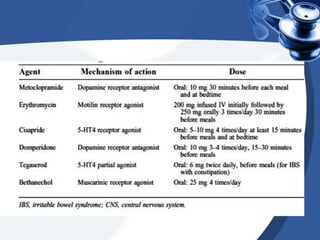
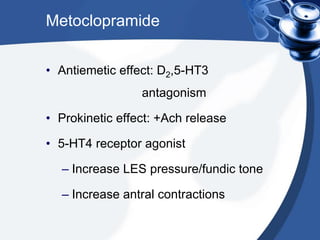
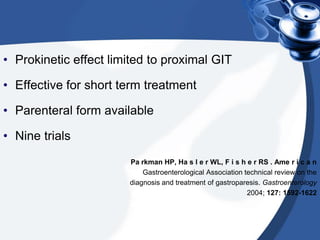
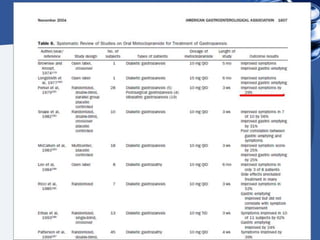
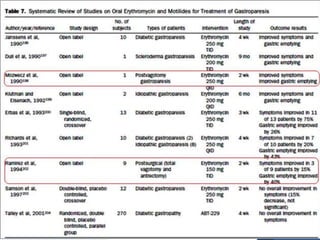
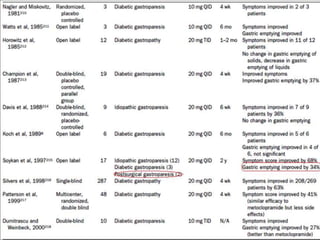
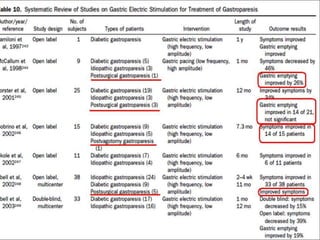
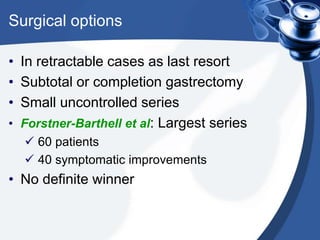
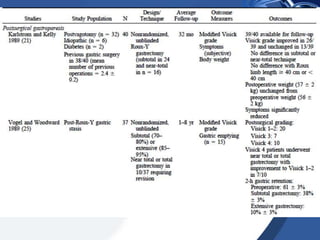
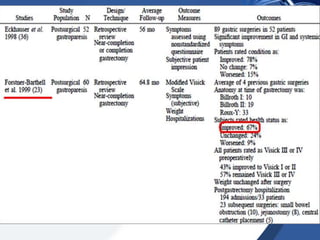
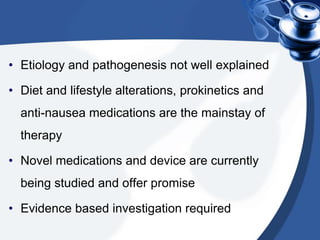
This document discusses post-surgical gastroparesis. It begins by describing a patient's presentation of nausea, vomiting and abdominal distension following surgery. It then covers the pathogenesis, clinical manifestations including nausea and bloating, evaluation using gastric emptying scans and wireless motility capsules, and treatment including prokinetic medications and dietary recommendations. Surgical options are mentioned as a last resort for refractory cases.