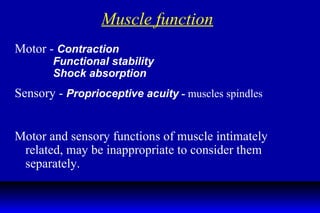
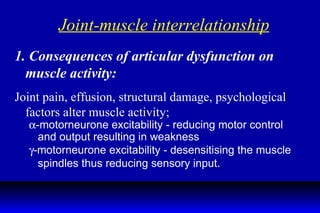
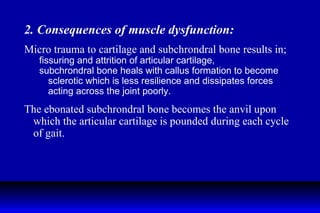
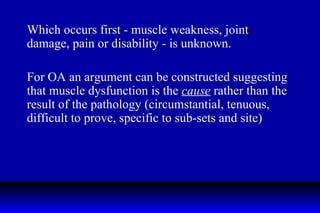
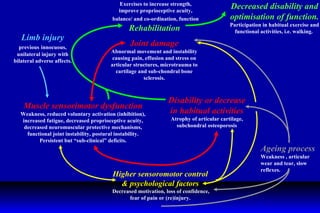
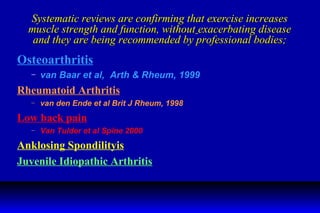
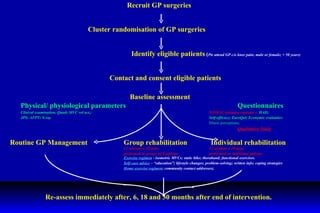
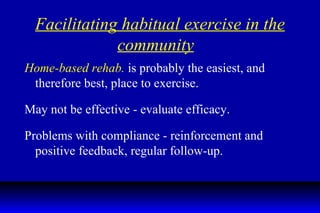
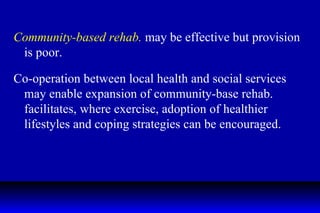
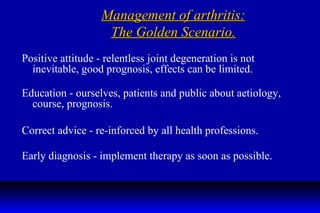
Muscle function and strength are vital for joint health and proper functioning. Muscle weakness and dysfunction may be an important factor in the development of joint damage in conditions like osteoarthritis. While the relationship between muscle and joint problems is complex, regular exercise and physical rehabilitation can help maintain muscle strength and proprioception, delaying or preventing further joint deterioration. Community- and home-based exercise programs are important for allowing patients to independently manage their condition long-term through regular physical activity.