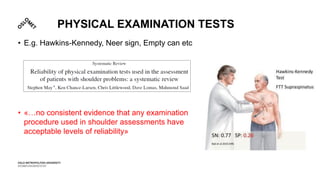
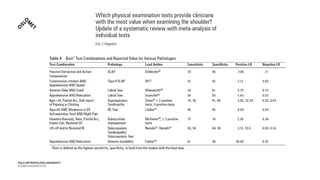
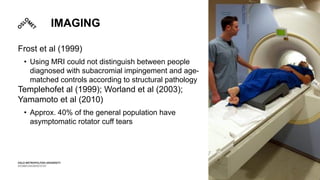
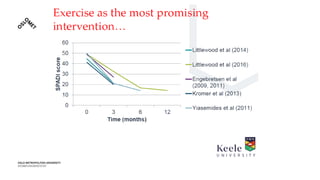
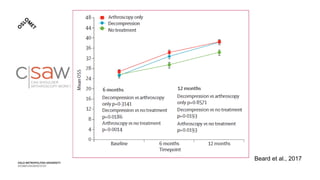
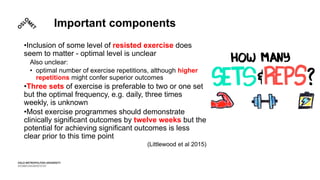
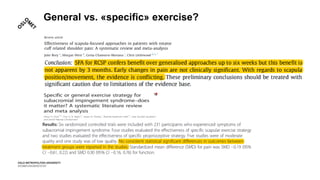
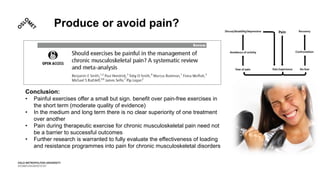
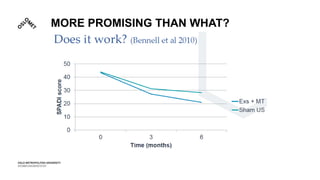
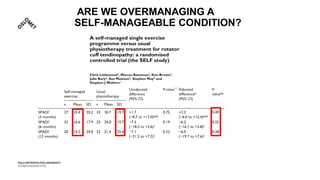
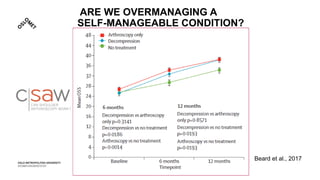
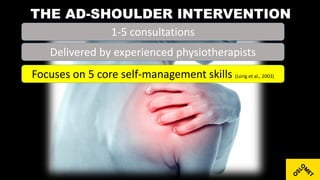
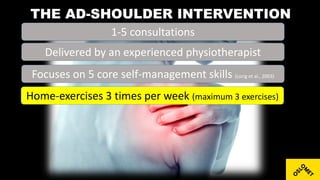
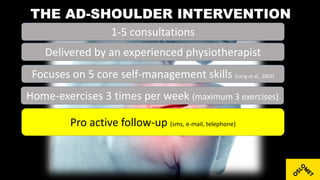
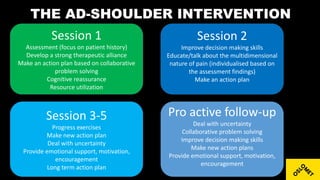
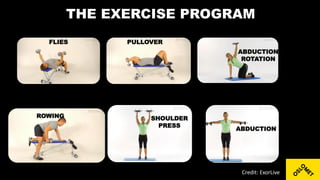
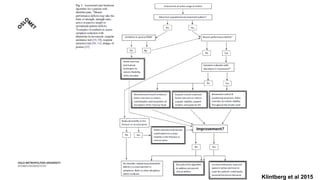
The document discusses shoulder pain, specifically subacromial pain/non-specific shoulder pain. It notes that shoulder pain is prevalent, can impact daily activities, and for 40% of patients the pain is ongoing or recurrent after 12 months. Imaging and physical exams are not always reliable in diagnosing the source of pain. Exercise appears to be the most promising intervention for shoulder pain, though what type or amount of exercise is unclear. A proposed intervention focuses on teaching patients self-management skills and a home exercise program with 1-5 sessions from a physiotherapist and proactive follow-up.