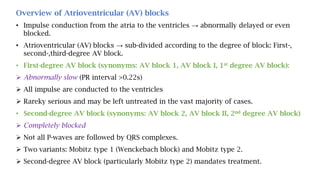
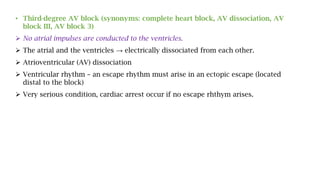
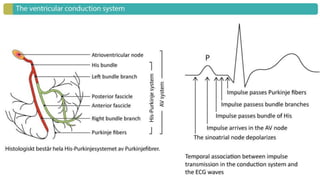
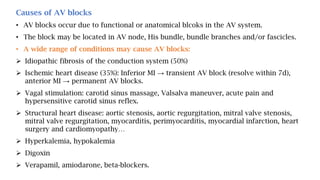
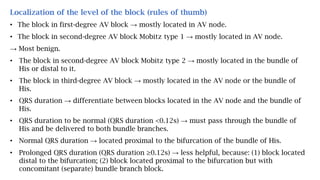
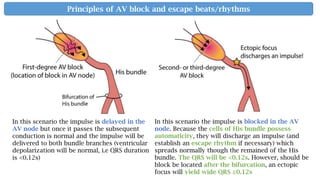
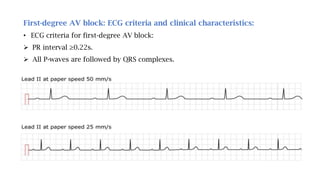
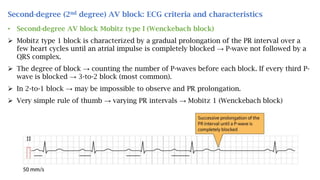
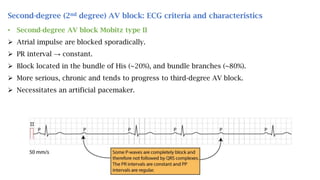
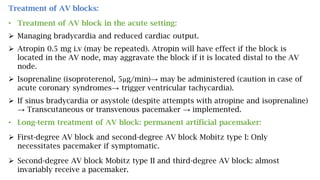
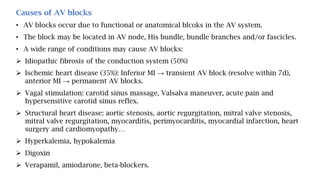
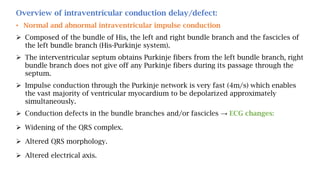
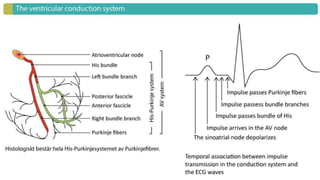
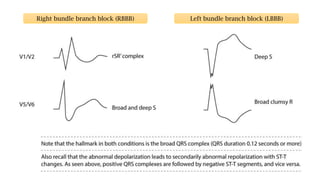
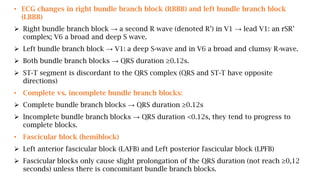
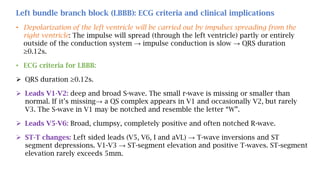
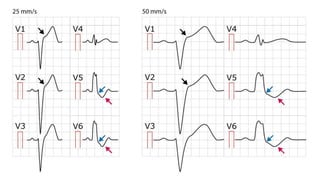
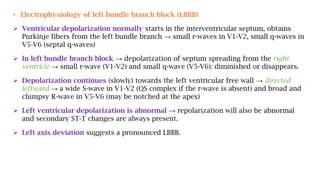
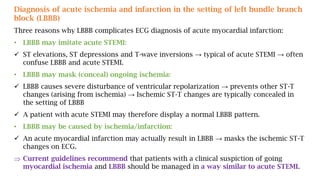
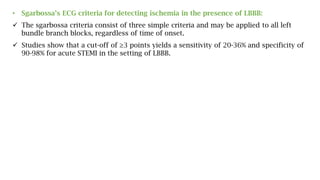
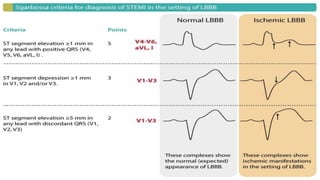
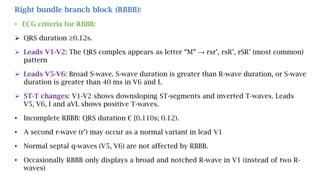
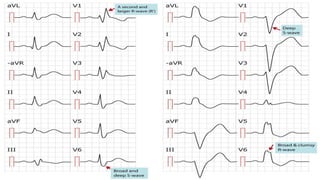
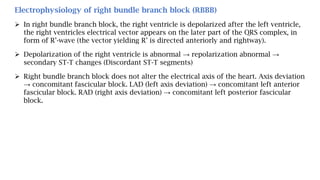
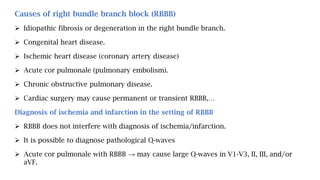
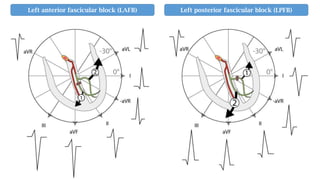
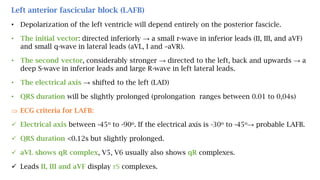
This document provides an overview of conduction defects (disturbances) including different types of atrioventricular (AV) blocks and intraventricular conduction delays. It describes the ECG criteria and characteristics of first-, second-, and third-degree AV blocks as well as right and left bundle branch blocks. Causes, clinical implications, localization, and treatment approaches for various conduction abnormalities are also discussed.