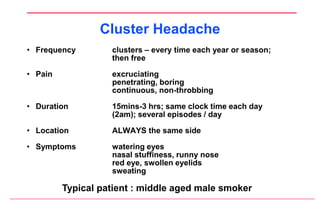
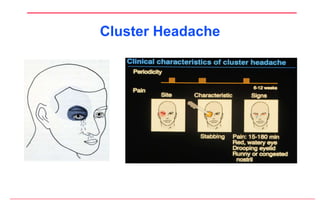
This document summarizes headache diagnosis and treatment. It begins by explaining that in most cases, headaches are not caused by brain damage but by issues with brain membranes and blood vessels. It then discusses the most common types of primary headaches like tension, migraine, and cluster headaches. The document outlines diagnosis methods and treatments for different headaches, including general pain relievers, triptans, ergots, and preventative medications. It concludes by discussing non-drug therapies and new research into non-drug electrical therapy, new drug approaches, and potential "vaccinations" for migraine prevention.