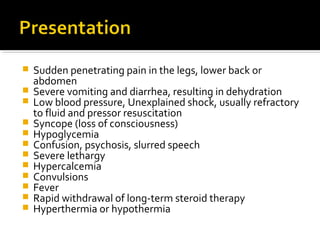
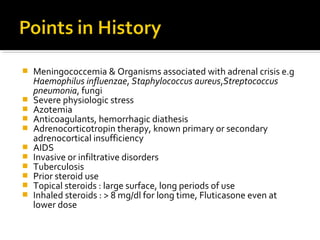
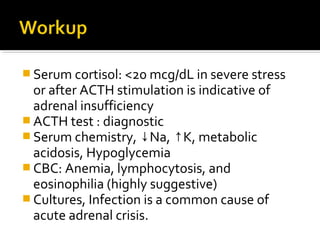
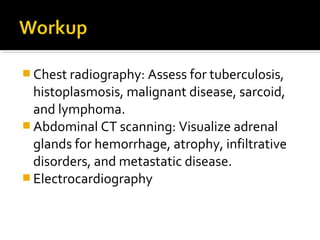
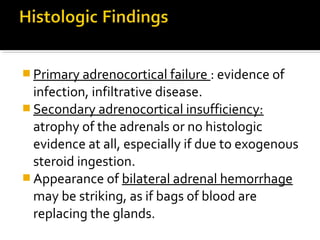
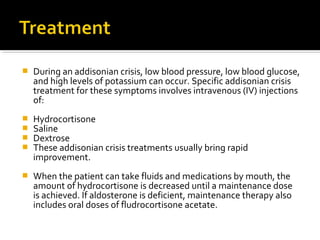
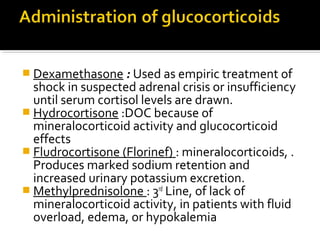
This document outlines the signs and symptoms of adrenal crisis including severe abdominal pain, vomiting, diarrhea, dehydration, low blood pressure, hypoglycemia and more. It then describes the diagnostic tests and findings including low cortisol levels, electrolyte abnormalities, and imaging. The treatment of adrenal crisis is also covered, focusing on intravenous hydrocortisone, saline, dextrose to address low blood pressure, blood glucose and potassium levels along with oral hydrocortisone and fludrocortisone as maintenance.