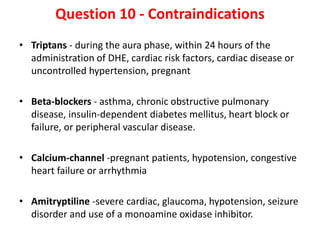
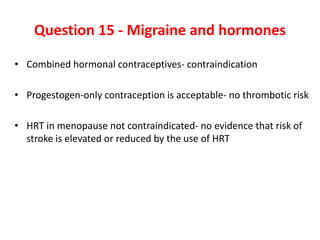
This document provides guidelines for the management and treatment of migraines. It discusses various drug options for acute/abortive treatment, preventative treatment, and treatment of refractory cases. It also addresses special considerations for medication overuse headache, menstrual migraine, and pregnancy-related migraine management. Non-pharmacological options including behavioral therapies and physical treatments are also summarized. Recent developments involving CGRP antagonists as a new drug class for migraine prevention are mentioned.