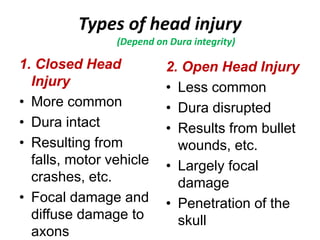
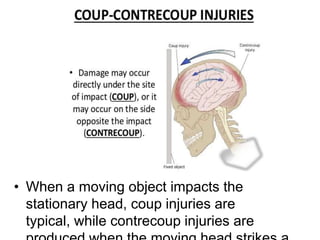
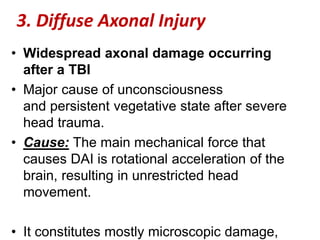
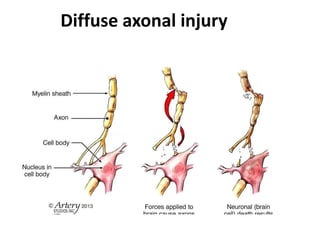
This document discusses traumatic brain injuries. It describes two main types of head injuries - closed head injuries where the dura is intact from falls or crashes, and open head injuries where the dura is disrupted by bullet wounds. Injuries can include skull fractures, damage to brain tissue, and vascular injuries like epidural, subdural, or intracerebral hemorrhages. The severity of brain damage depends on factors like the force of impact and whether the head is moving. Diffuse axonal injury is widespread axonal damage that can cause unconsciousness.