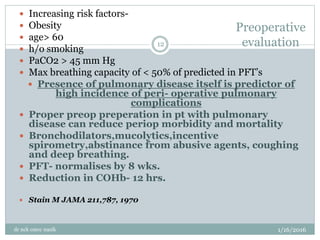
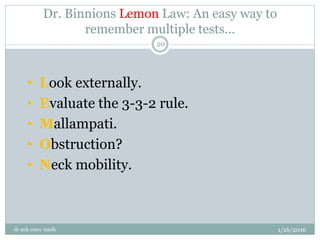
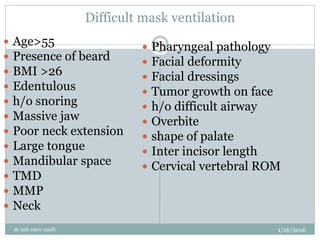
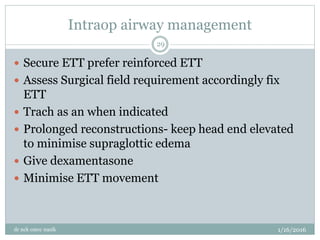
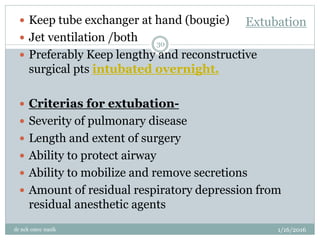
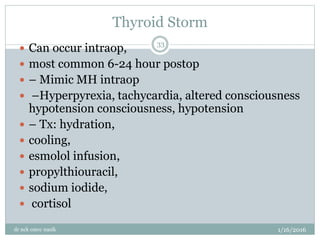
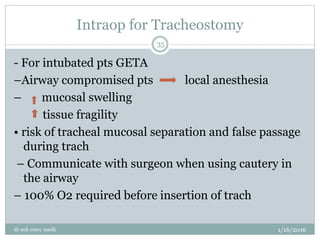
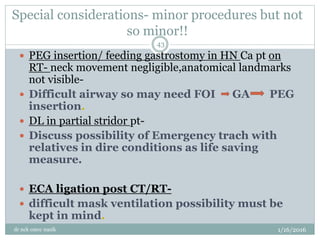
The document outlines the anesthetic considerations and peri-operative management for patients undergoing head and neck cancer surgeries. It highlights the epidemiology of head and neck cancers, risk factors, anesthetic management strategies, and specific challenges associated with airway management in these patients. Additionally, it discusses the implications of age, cancer treatment, and preoperative evaluations on surgical outcomes.