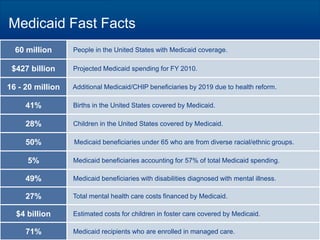
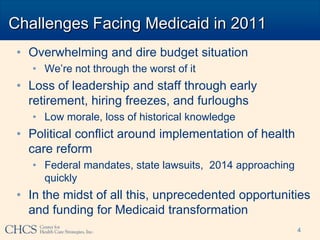
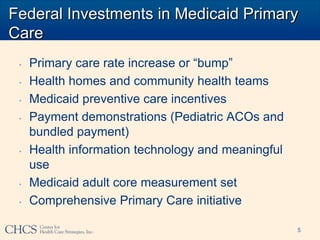
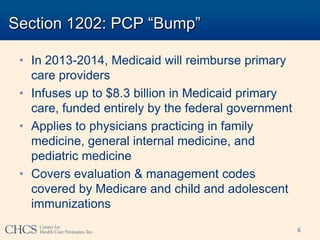
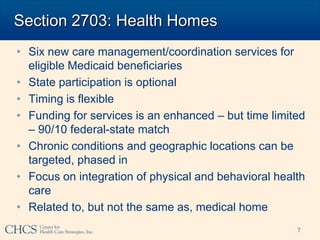
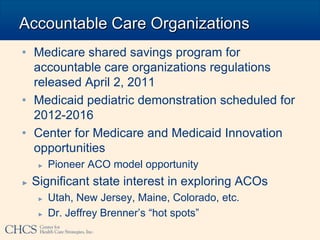
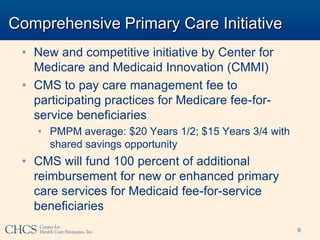
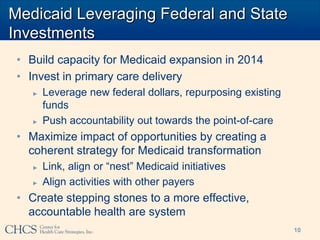
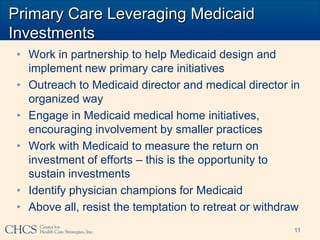
This document discusses recent federal investments in Medicaid primary care and opportunities for states to leverage these investments. It outlines initiatives like the primary care rate increase, health homes, and accountable care organizations that provide funding for services. The document urges working in partnership with Medicaid to help design and implement these initiatives, engage providers, measure returns on investment, and identify physician champions to sustain the investments and strengthen primary care.