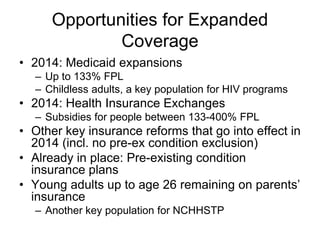
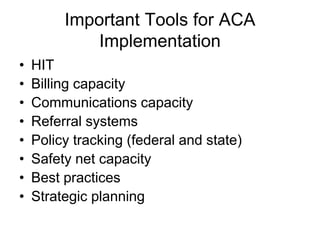
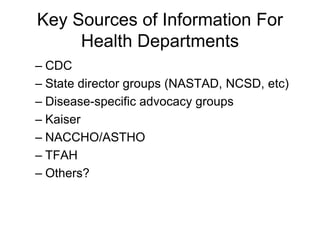
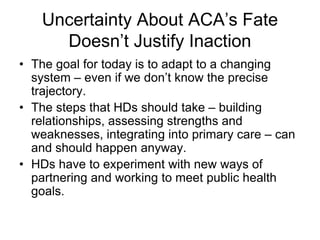
This document summarizes key opportunities and threats to public health from recent health reform efforts. It outlines threats from potential budget cuts at state and federal levels. It also outlines opportunities from expanded insurance coverage through Medicaid expansions and health insurance exchanges in 2014. Specifically, it discusses opportunities for better coverage of preventive services, essential community providers, and integration into the primary care system. The document urges public health departments to build relationships and prepare tools to capitalize on reforms and ensure continued support for public health programs, despite ongoing uncertainties.