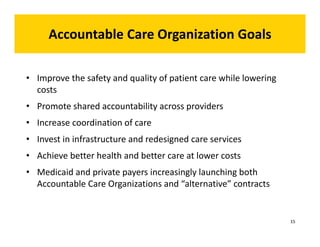
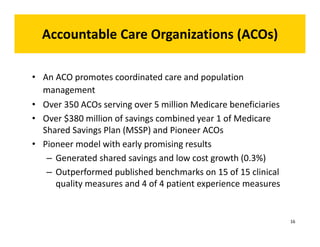
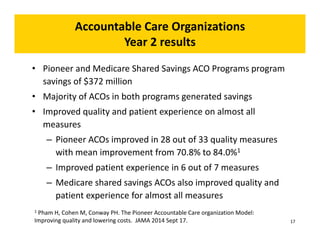
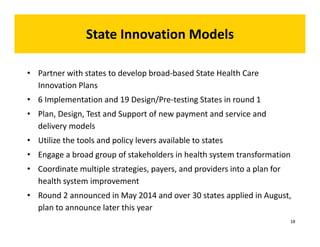
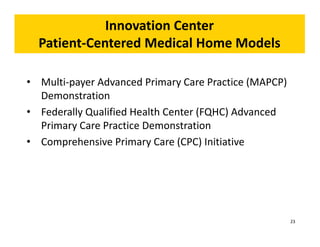
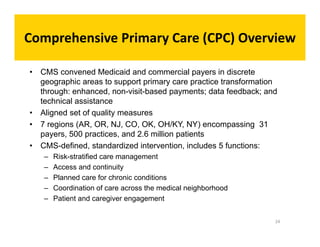
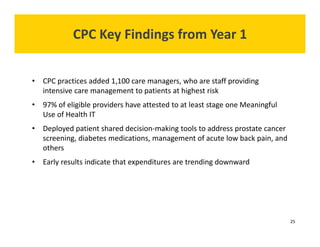
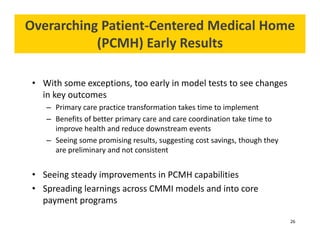
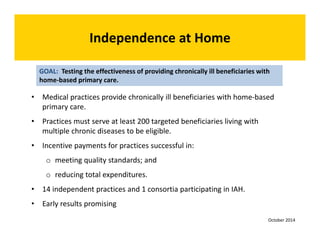
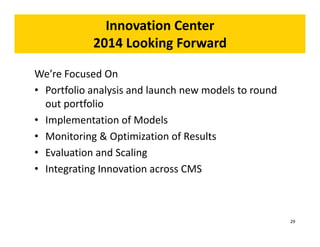
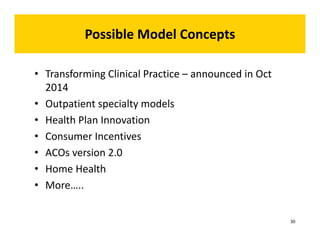
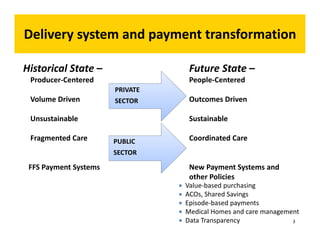
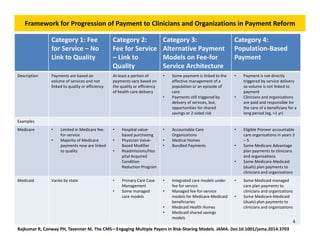
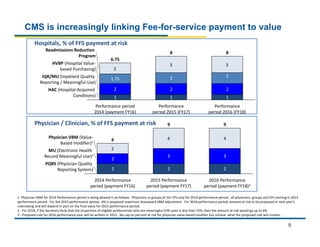
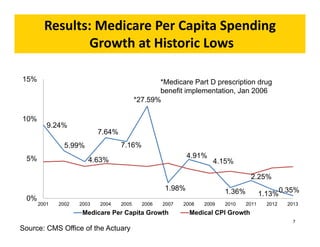
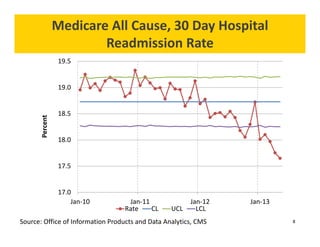
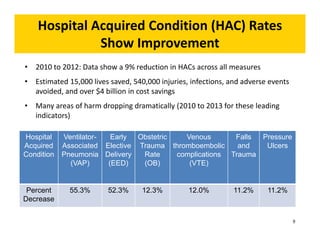
The document discusses the Center for Medicare and Medicaid Innovation's efforts to reform payment and service delivery models to enhance quality of care while reducing costs. It highlights various payment models, such as value-based purchasing and accountable care organizations (ACOs), and reviews early results demonstrating improvements in quality metrics and cost reduction. Additionally, it outlines future directions for innovation and the importance of integrating new models within CMS operations.


![The purpose of the [Center] is to test innovative
payment and service delivery models to reduce program
expenditures…while preserving or enhancing the quality
of care furnished to individuals under such titles.
- The Affordable CareAct
Identify, Test, Evaluate, Scale
The CMS Innovation Center
11](https://image.slidesharecdn.com/cmsinnovationcenter-updatewebinarwpatrick111014-141110110917-conversion-gate01/85/Webinar-CMS-Innovation-Center-Update-11-320.jpg)