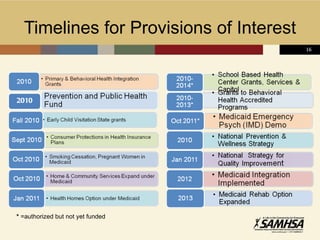
The Affordable Care Act will significantly expand access to healthcare coverage and improve health outcomes over the next few years, especially for those with behavioral health needs. Key provisions include expanding Medicaid eligibility and establishing health insurance exchanges. This will reduce the number of uninsured Americans, including many who are currently unable to access behavioral healthcare. The changes brought about by the ACA will disproportionately benefit rural communities, where access to insurance and services is more limited. Full implementation will occur in phases over several years to allow for development of new infrastructure and systems.