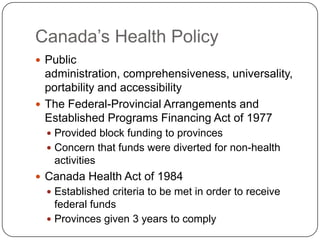
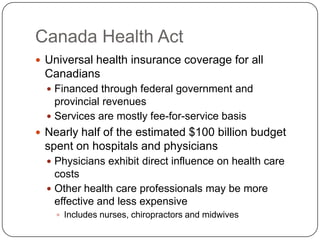
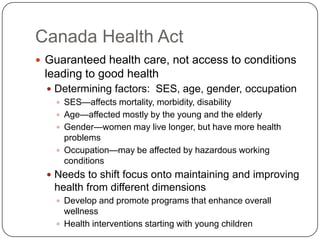
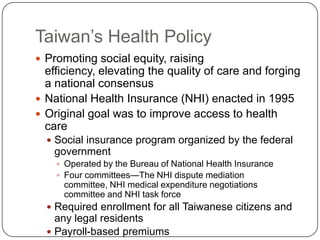
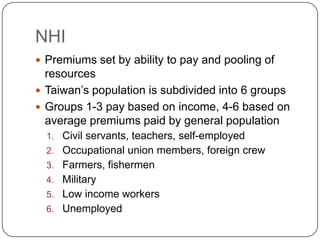
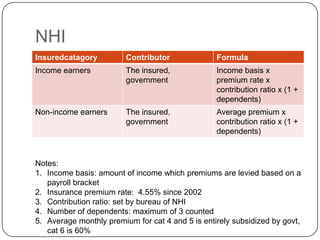
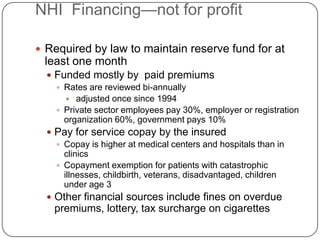
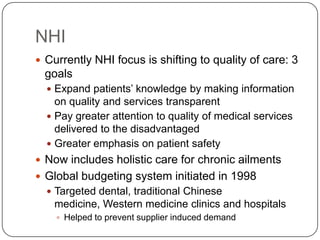
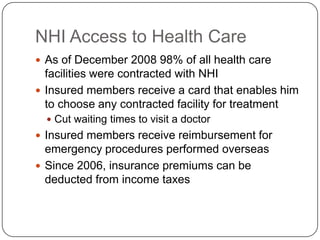
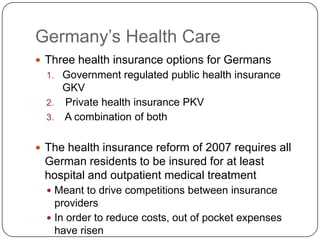
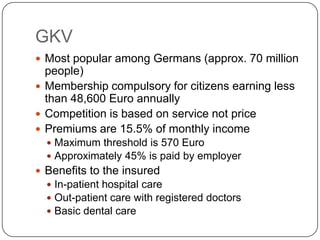
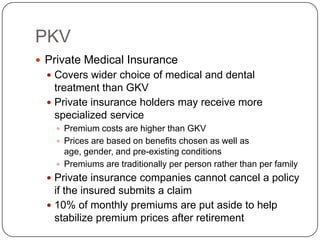
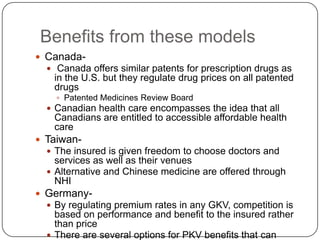
The document discusses and compares the health care policies of Canada, Taiwan, and Germany. Canada's single-payer system is funded through federal and provincial revenues and guarantees universal coverage. Taiwan implemented its National Health Insurance program in 1995 to improve access through a social insurance model with premiums based on income. Germany offers public and private health insurance options, with most citizens covered by the mandatory not-for-profit public option regulated to focus on service rather than price competition.