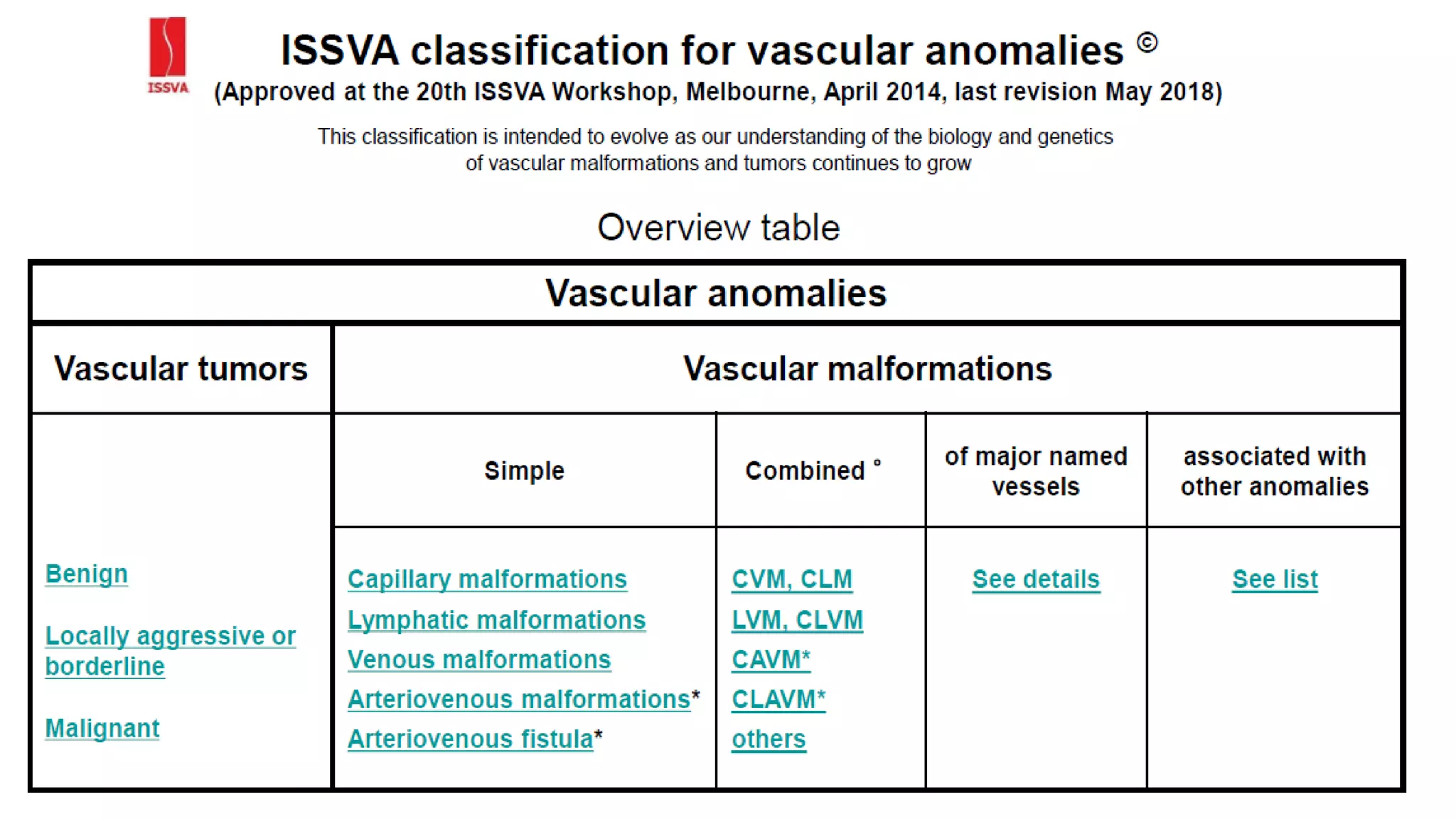
Vascular malformations are abnormalities of blood or lymph vessels that are present at birth. They can involve arteries, veins or lymphatics. There are several classifications including anatomical, biological, and ISSVA classifications. Vascular malformations are caused by arrested development of blood vessels during embryogenesis. Common types include capillary, venous, arterial and lymphatic malformations. Clinical features, investigations, and treatment options vary depending on the type of malformation and include sclerotherapy, laser therapy, surgery, and embolization. Complications can include bleeding, infection, and pressure effects on surrounding structures.