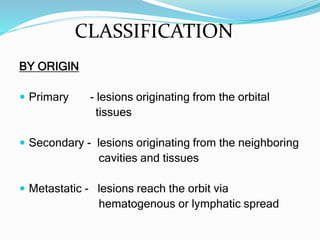
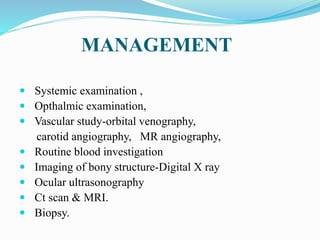
Orbital tumors can be primary, secondary, or metastatic in origin. The most common malignant orbital tumor in adults is lymphoma, which typically involves the lacrimal gland. Malignant melanoma of the uvea is also relatively common and can arise in the iris, ciliary body, or choroid. Treatment options depend on the type and size of the tumor but may include surgery, radiation therapy such as plaque brachytherapy, proton beam therapy, or stereotactic radiotherapy. Complications can include vision loss, glaucoma, and cataracts.