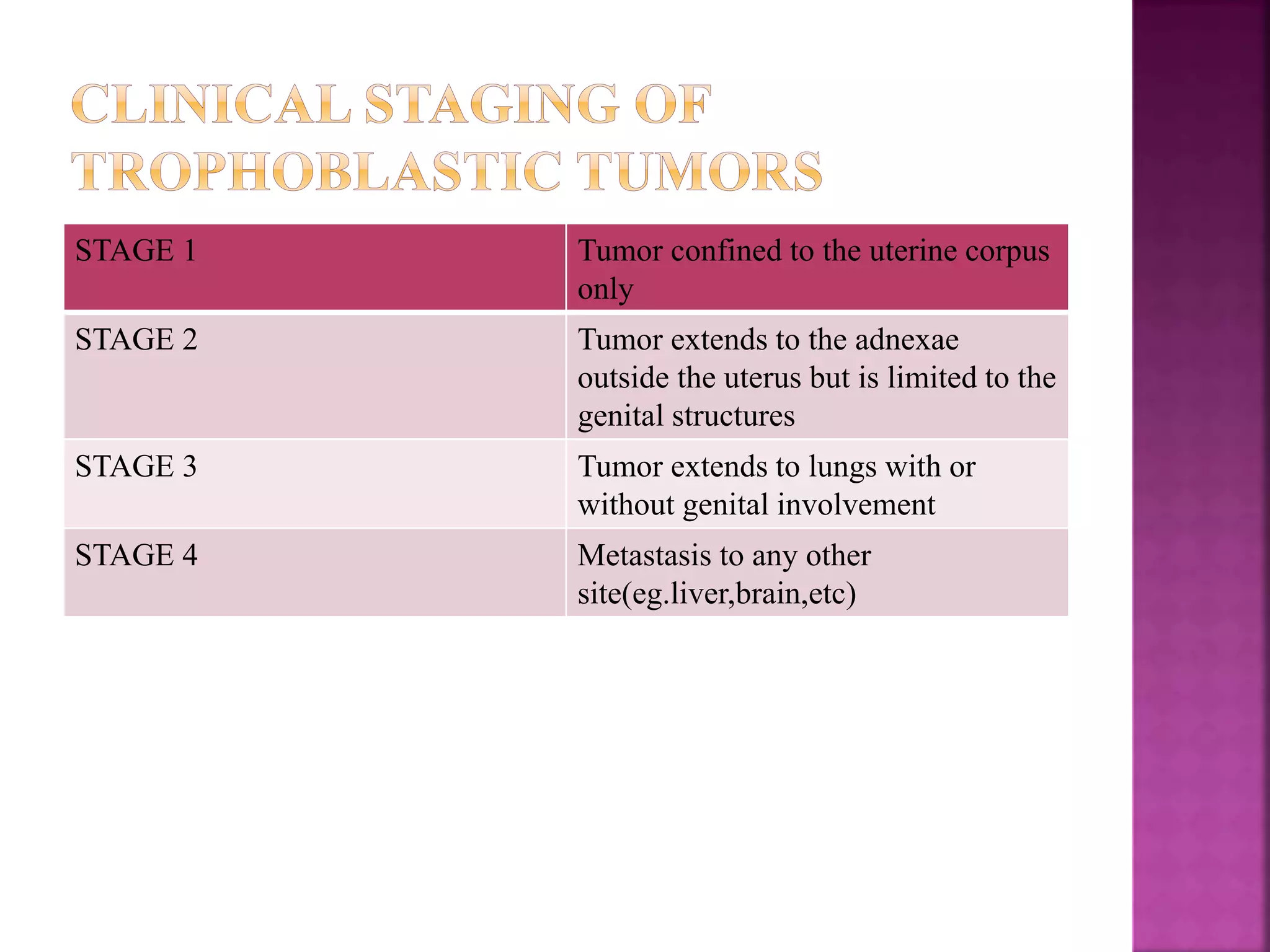
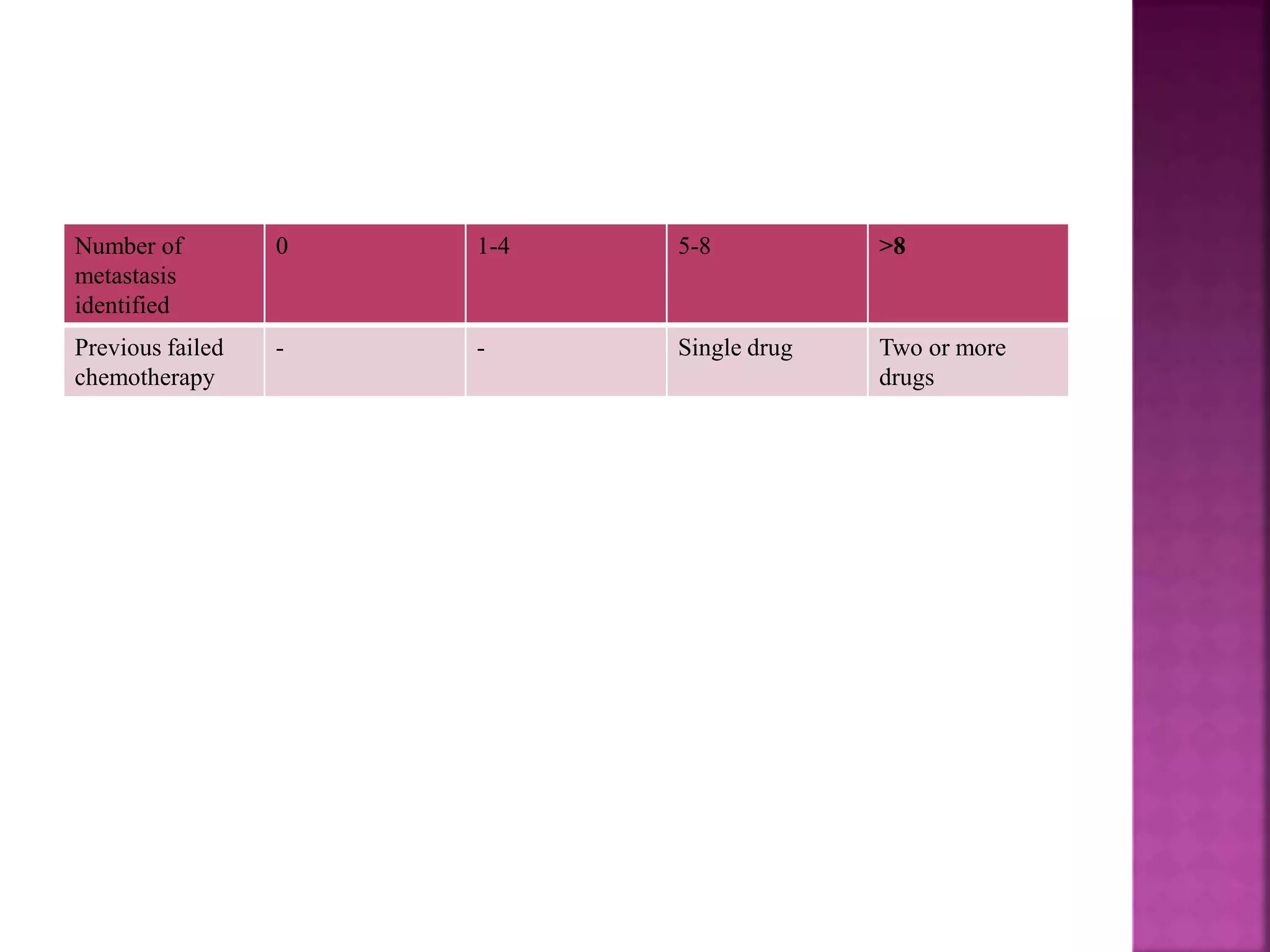
This document discusses gestational trophoblastic tumors including invasive mole, choriocarcinoma, and placental site trophoblastic tumor. Invasive mole can progress to choriocarcinoma but may also regress spontaneously. Choriocarcinoma arises from the chorionic epithelium and has markedly elevated beta-HCG levels. Staging and prognostic scoring is described for choriocarcinoma. Low and high risk disease is defined and different chemotherapy regimens are outlined depending on the risk level. Exceptions for chemotherapy include invasive mole perforating the serosa or uncontrollable bleeding.