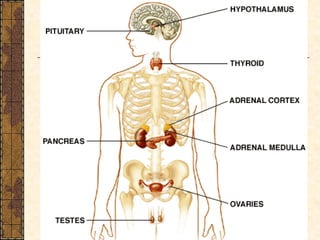
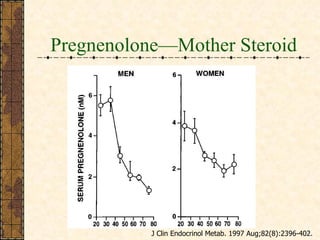
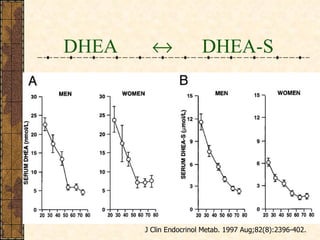
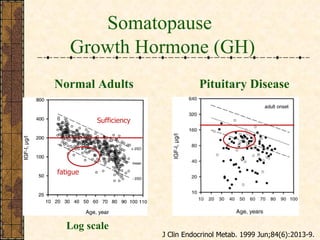
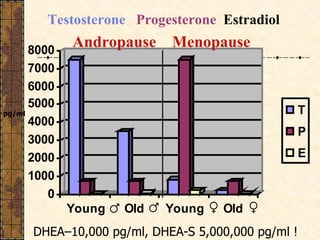
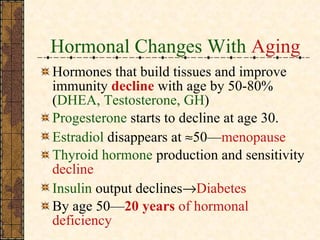
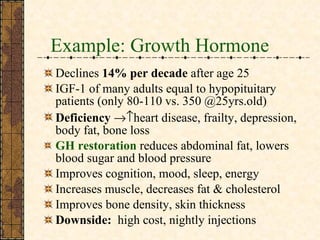
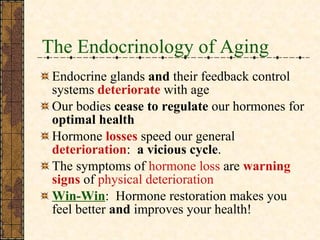
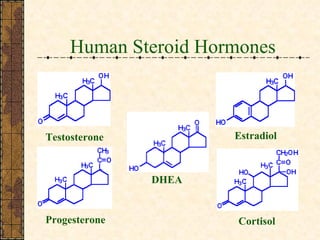
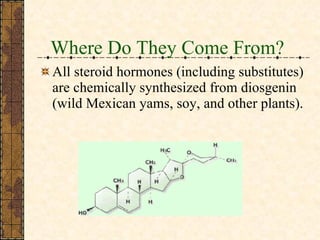
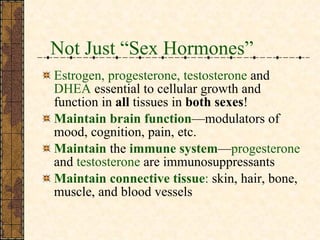
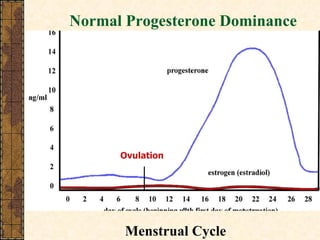
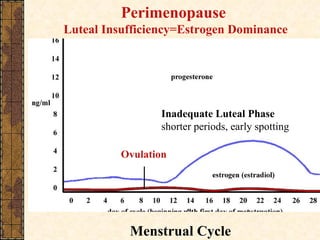
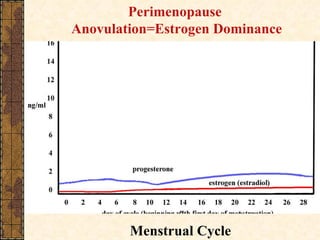
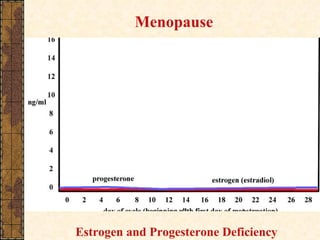
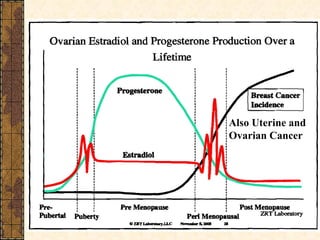
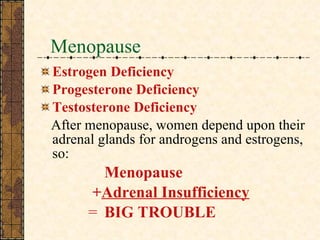
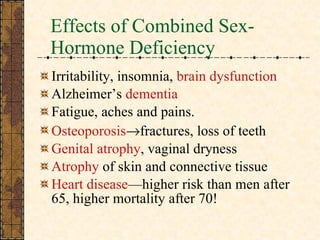
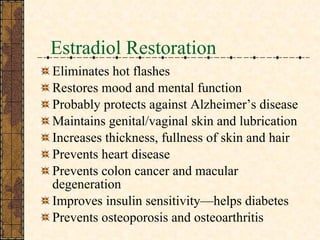
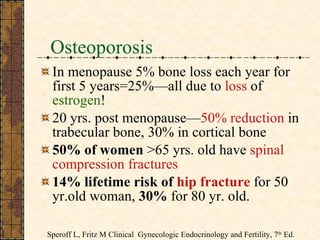
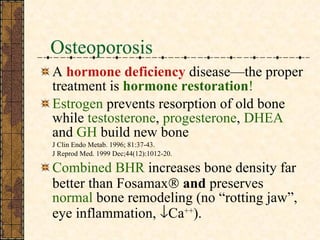
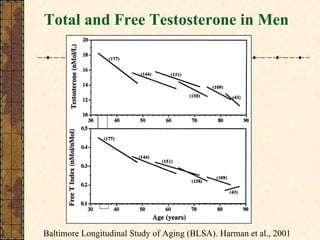
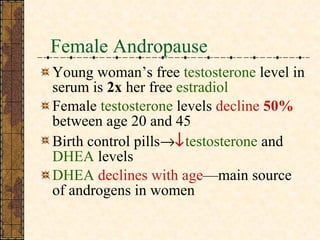
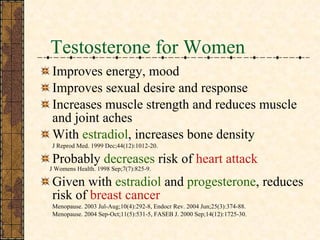
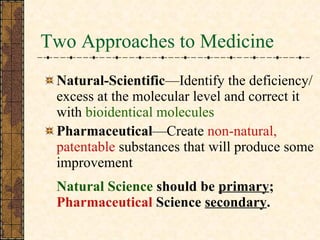
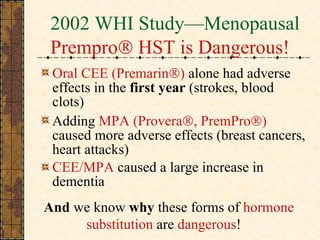
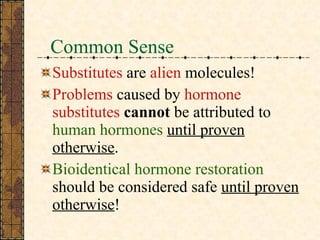
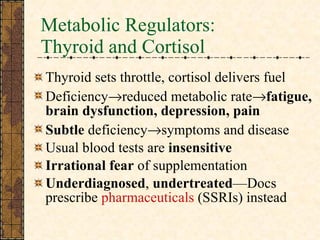
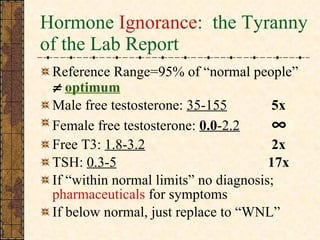
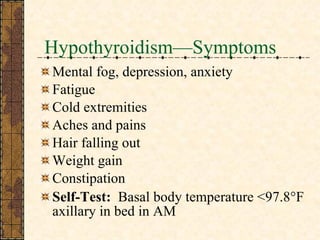
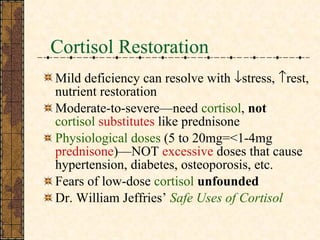
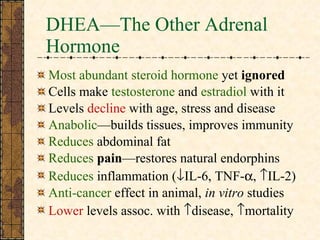
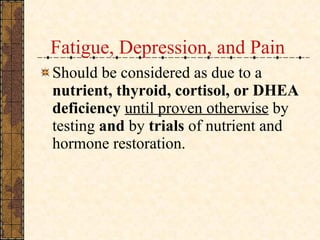
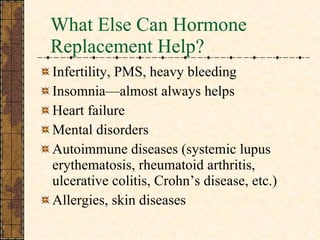
The document discusses bioidentical hormone restoration as a means to replace hormones lost due to aging. It argues that losing hormones is not adaptive and leads to various health issues. Restoring youthful hormone levels through bioidentical replacements can improve health, prevent disease, and enhance quality of life by treating symptoms caused by hormone deficiencies. Common hormones that decline with age include testosterone, growth hormone, DHEA, progesterone, and estrogen.

![For More Information The Miracle of Natural Hormones David Brownstein, MD How to Achieve Healthy Aging—Look, Live, and Feel Fantastic After 40 Neal Rouzier, MD The Hormone Solution—Stay Younger Longer Thierry Hertoghe, MD Life Extension Foundation (www.lef.org) BHRT info. and hundreds of abstracts at www.hormonerestoration.com . Contact me: [email_address]](https://image.slidesharecdn.com/bioidenticalornaturalhormonereplacementtherapy-110813232539-phpapp01/85/Bio-Identical-or-Natural-Hormone-Replacement-Therapy-98-320.jpg)