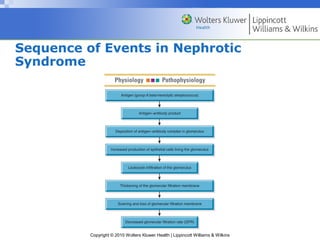
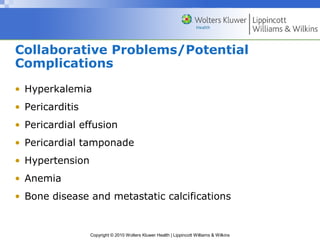
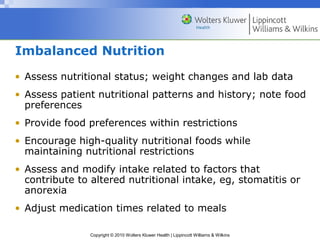
The document discusses renal disorders including causes and management of acute and chronic renal failure, glomerular diseases, and dialysis options. It covers nursing management of patients with renal disorders focusing on fluid balance, nutrition, education, and preventing complications like electrolyte imbalances. Surgical procedures for kidney problems and post-operative care are also reviewed.