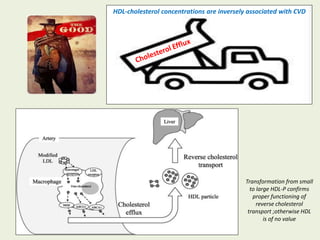
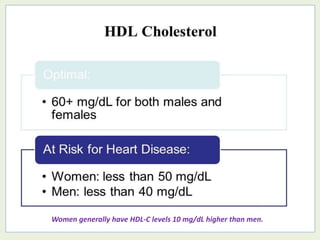
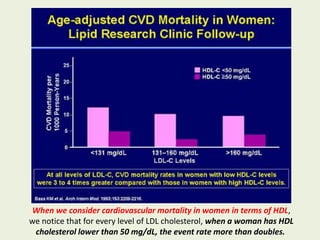
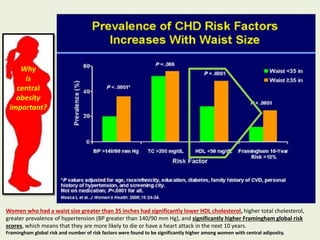
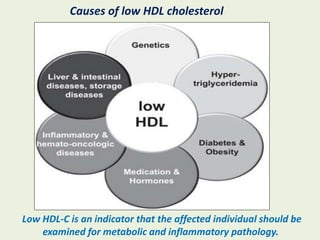
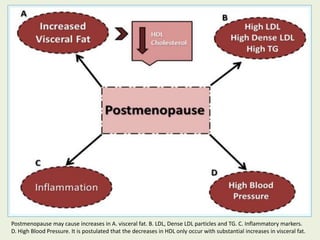
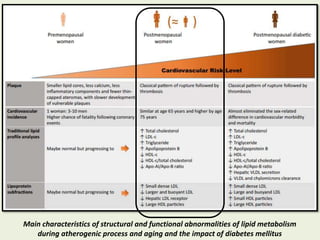
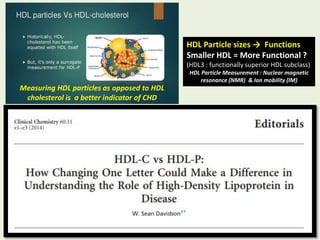
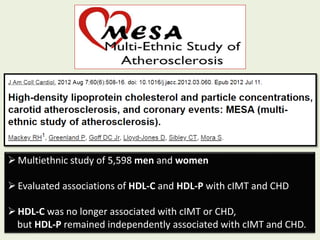
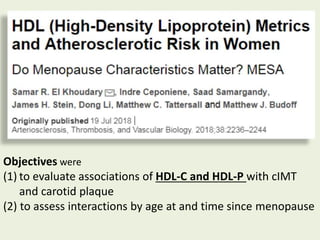
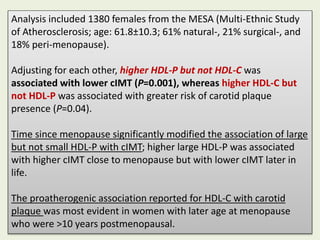
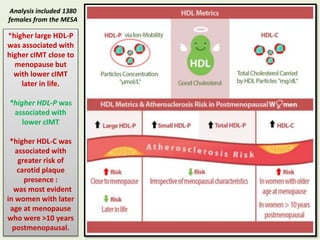
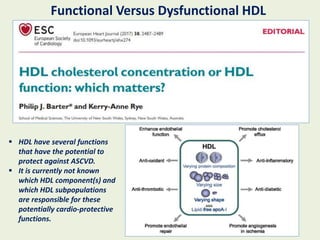
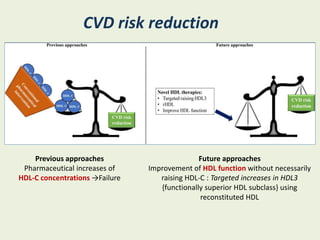
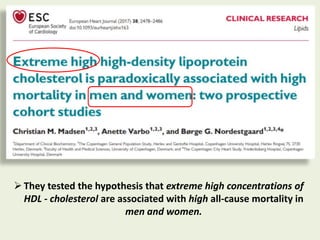
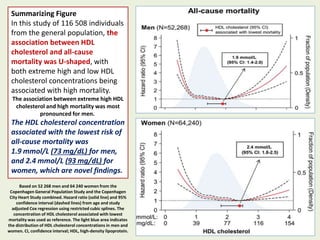
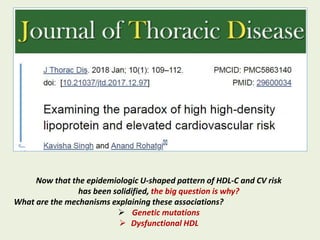
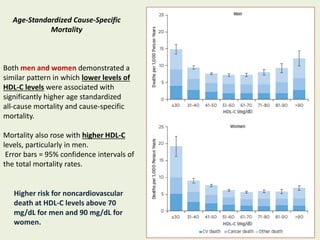
The document discusses a paradigm shift in understanding 'good cholesterol,' highlighting research that shows the relationship between HDL cholesterol and cardiovascular disease risk. It emphasizes the significance of HDL particle measurement over HDL cholesterol levels, noting that higher HDL particles are associated with lower carotid intima-media thickness (CIMT) and that extremes of HDL cholesterol levels correlate with increased mortality. Furthermore, the findings reveal a U-shaped association between HDL cholesterol concentrations and all-cause mortality, indicating potential mechanisms such as genetic mutations and dysfunctional HDL.