1. Glucose-6-phosphate dehydrogenase (G6PD) deficiency is the most common enzyme deficiency in humans, affecting over 200 million people worldwide.
2. G6PD deficiency results from mutations in the G6PD gene and causes decreased production of NADPH, leading to hemolytic anemia in response to oxidative stress.
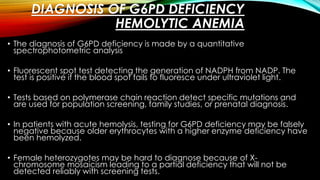
3. Diagnosis is made through tests that measure G6PD enzyme activity levels in red blood cells, with deficiency diagnosed if levels are significantly decreased. Management focuses on avoiding triggers that cause hemolysis and blood transfusions in acute cases.