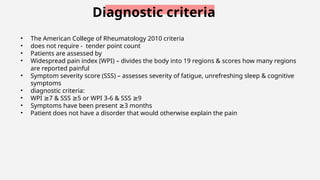
The document provides a comprehensive overview of fibromyalgia, including its introduction, epidemiology, etiology, pathophysiology, clinical presentation, diagnostic criteria, and management strategies. Key points highlight the condition's prevalence, particularly among women, and the significant impact it has on quality of life, emphasizing the importance of physiotherapy and multidisciplinary approaches in treatment. Various treatment options are discussed, including exercise, dietary management, and alternative therapies, all aimed at improving symptoms and overall well-being.

![Physiotherapy assessment
(Santos MR dos, Moro CMC, Vosgerau DSR. Protocolo para avaliação física em portadores de
síndrome de fibromialgia. Rev Bras Reumatol [Internet]. 2014Mar;54(2):117–23. Available from:
https://doi.org/10.1016/j.rbr.2014.03.006 )
History & pain assessment
Body composition: BMI and
bioimpedance
Cardiorespiratory capacity: 6-
minute walk.
Muscular strength and
endurance: Grip strength
(dynamometer), isometric force
apparatus, 30-second sit to stand
from a chair test, and 1 RM test
Flexibility: sit and reach test and
shoulder flexibility.
Balance and agility: Up and Go
test (dynamic balance and motor
agility) and flamingo balance
(static balance)](https://image.slidesharecdn.com/fibromyalgia-240802174702-d4f5eafd/85/Fibromyalgia-introduction-assessment-physiotherapy-management-pptx-12-320.jpg)




![Alternative management
• Education/Self-Guided Treatments:
• Because the etiology, diagnosis, and treatment of FM are often
misunderstood, proper education and self-management are essential
• FM Self-Help Course (FSHC)
• Cognitive-Behavioral Therapies:
• beliefs, thoughts, and perceptions – how these affect condition
• restructuring, prioritization, and goal setting are utilized to repattern
behavior
• Biofeedback:
• Pt have - autonomic dysfunction
• techniques or sensors to es mind-body awareness - muscle tension
↑
(sEMG) or autonomic tone [peripheral temperature, heart rate
variability (HRV), galvanic skin response] – can be modified, es
↑
awareness and es autonomic overarousal
↓
• depression and pain, functional status - es
↑](https://image.slidesharecdn.com/fibromyalgia-240802174702-d4f5eafd/85/Fibromyalgia-introduction-assessment-physiotherapy-management-pptx-22-320.jpg)