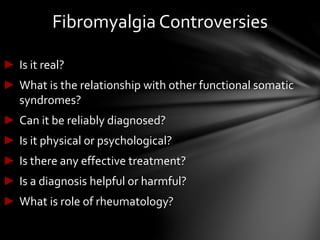
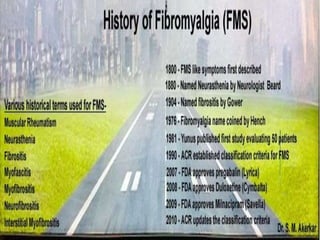
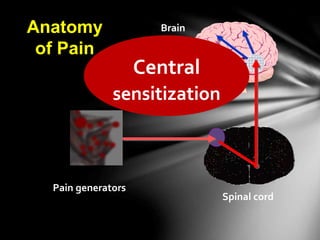
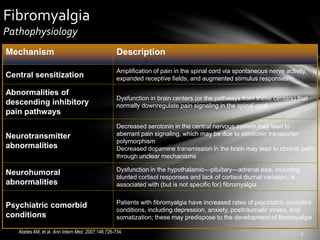
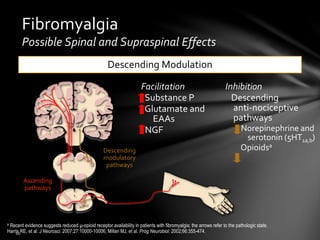
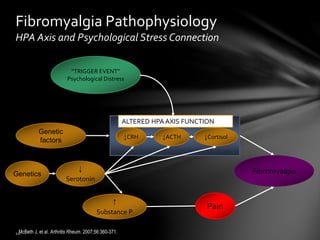
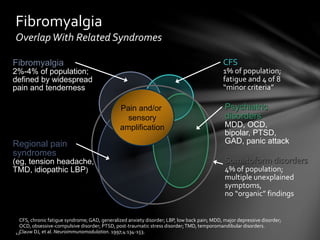
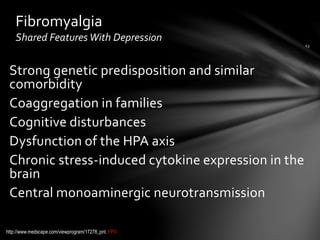
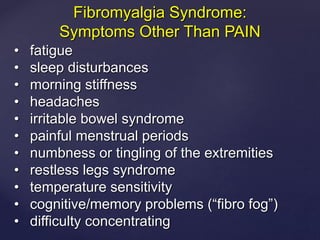
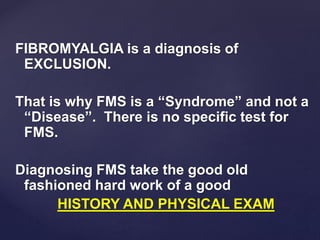
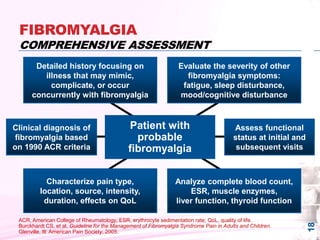
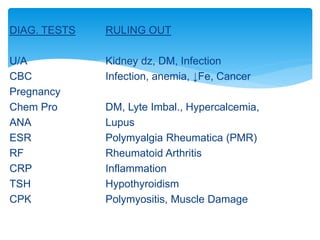
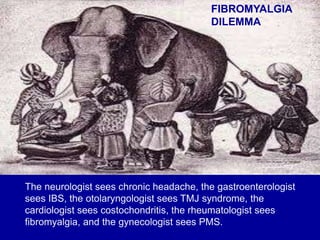
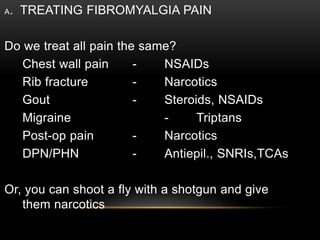
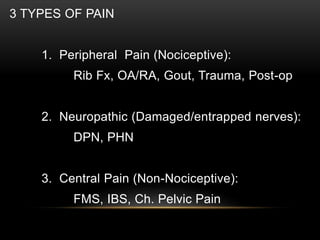
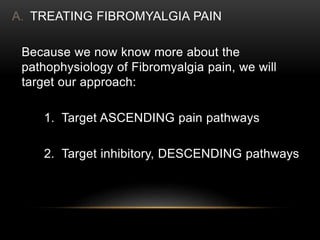
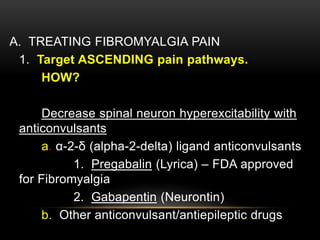
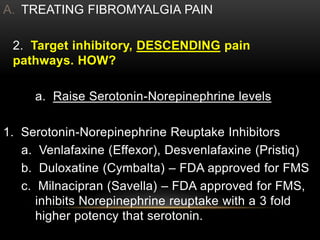
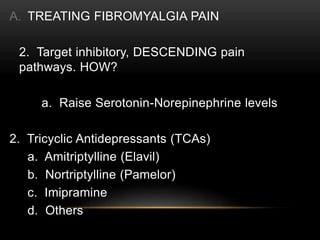
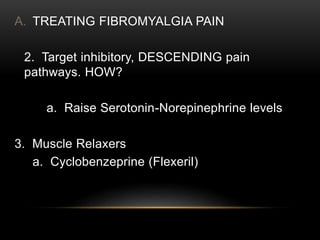
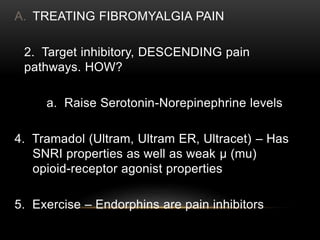
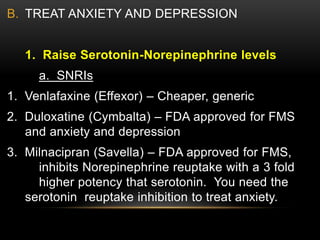
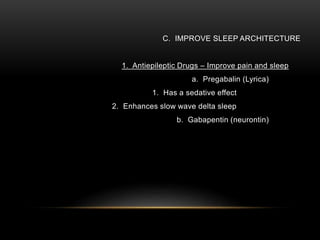
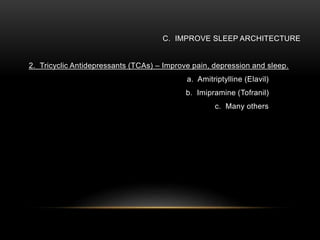
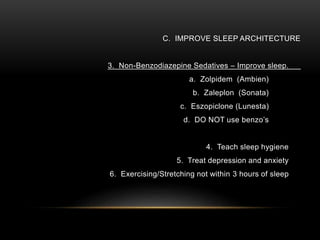
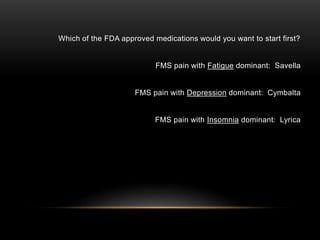
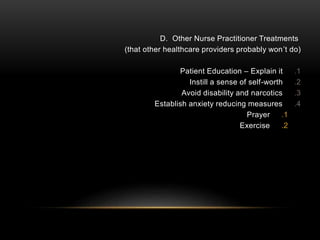
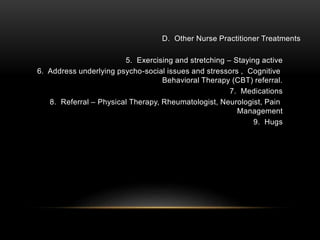
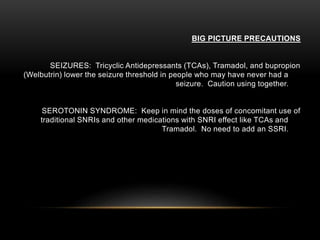
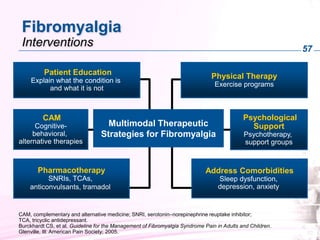
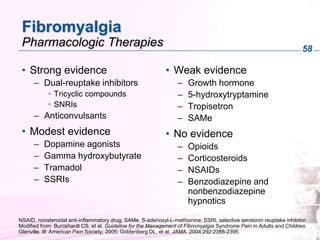
The document discusses fibromyalgia syndrome, emphasizing the challenges of diagnosing and treating the condition. It covers the pathophysiology, potential causes, and treatment strategies, including medications and lifestyle modifications. Additionally, it highlights the importance of comprehensive assessments to identify comorbidities and tailor treatment plans for effective pain management.