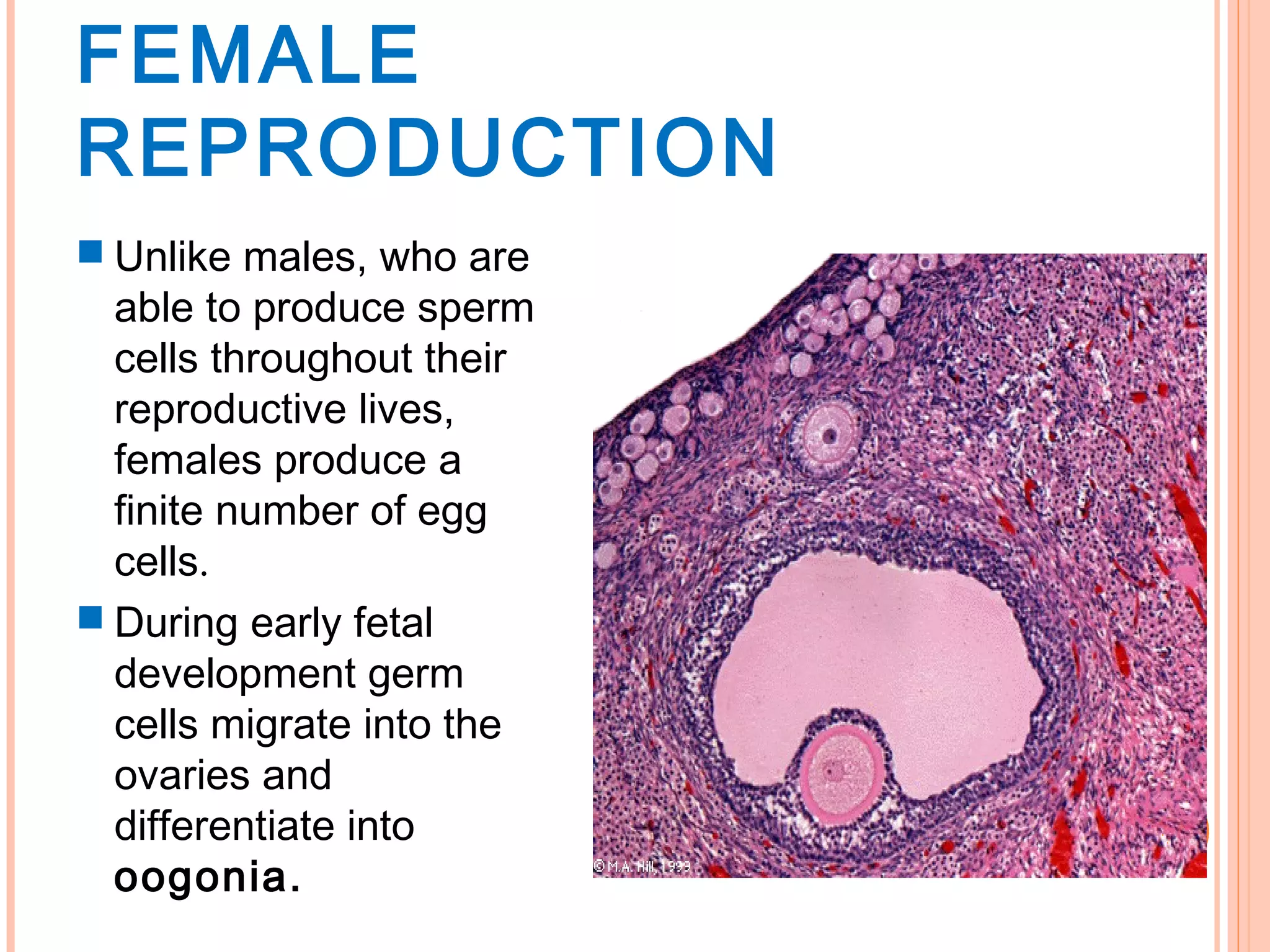
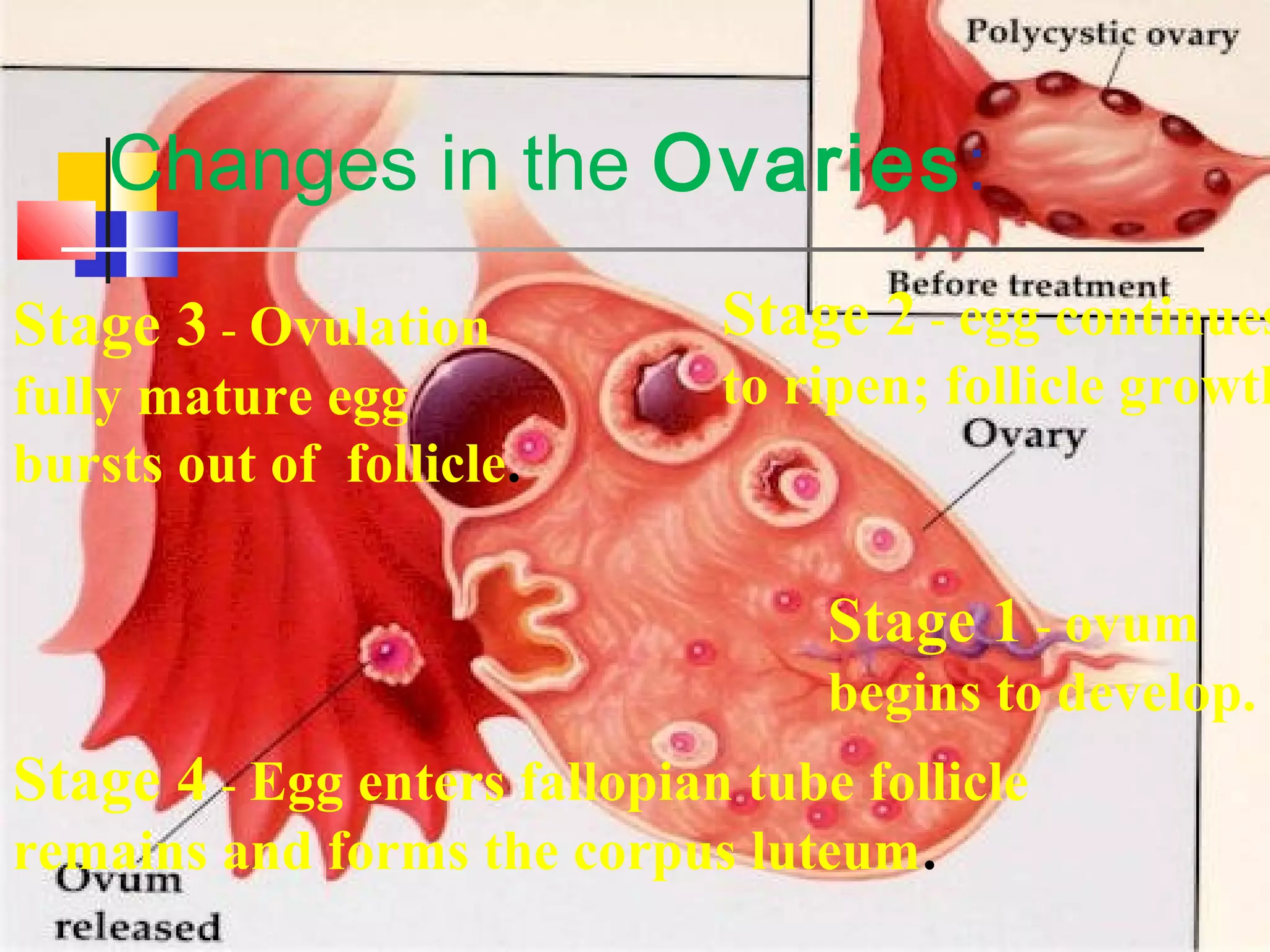
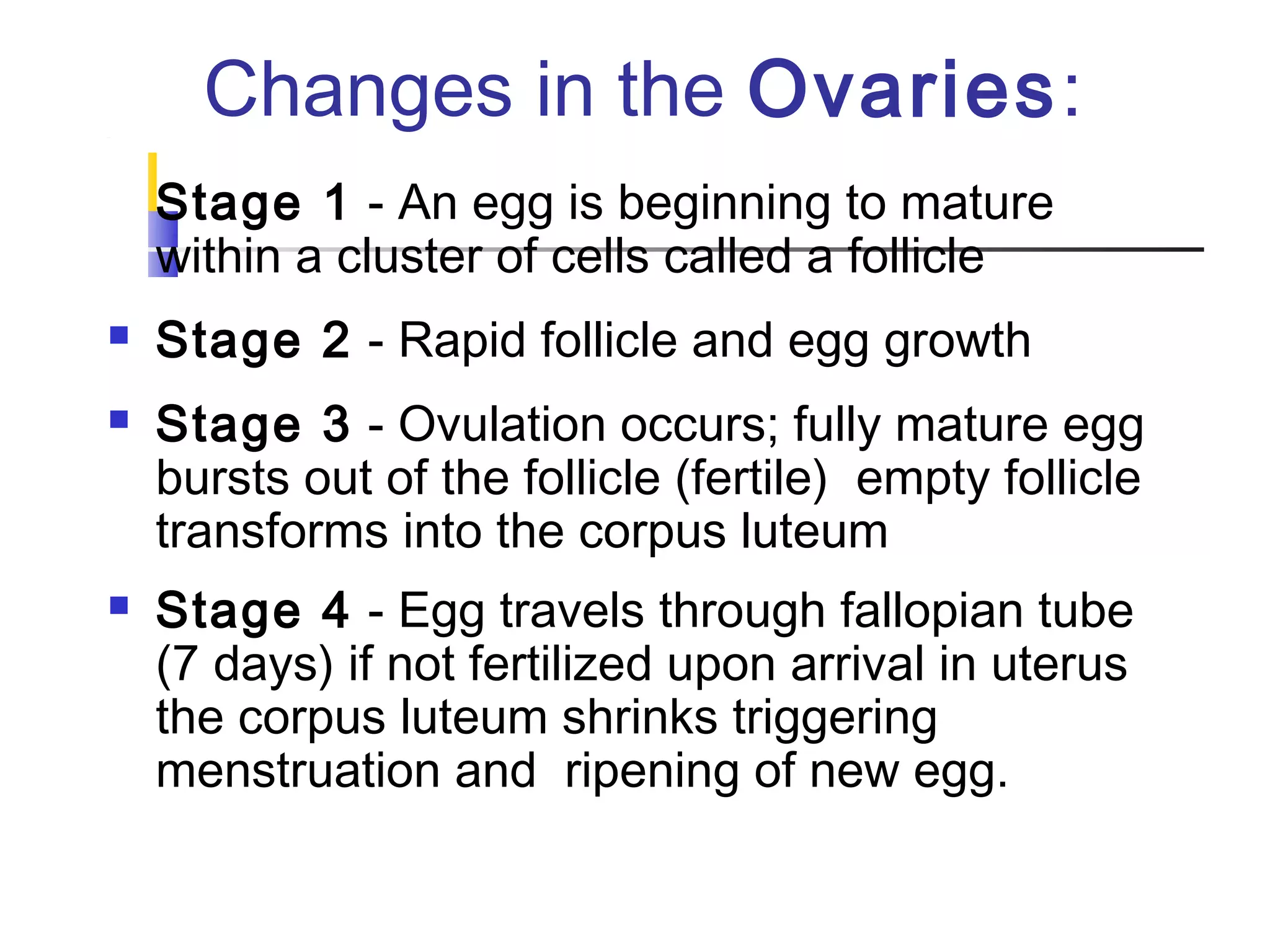
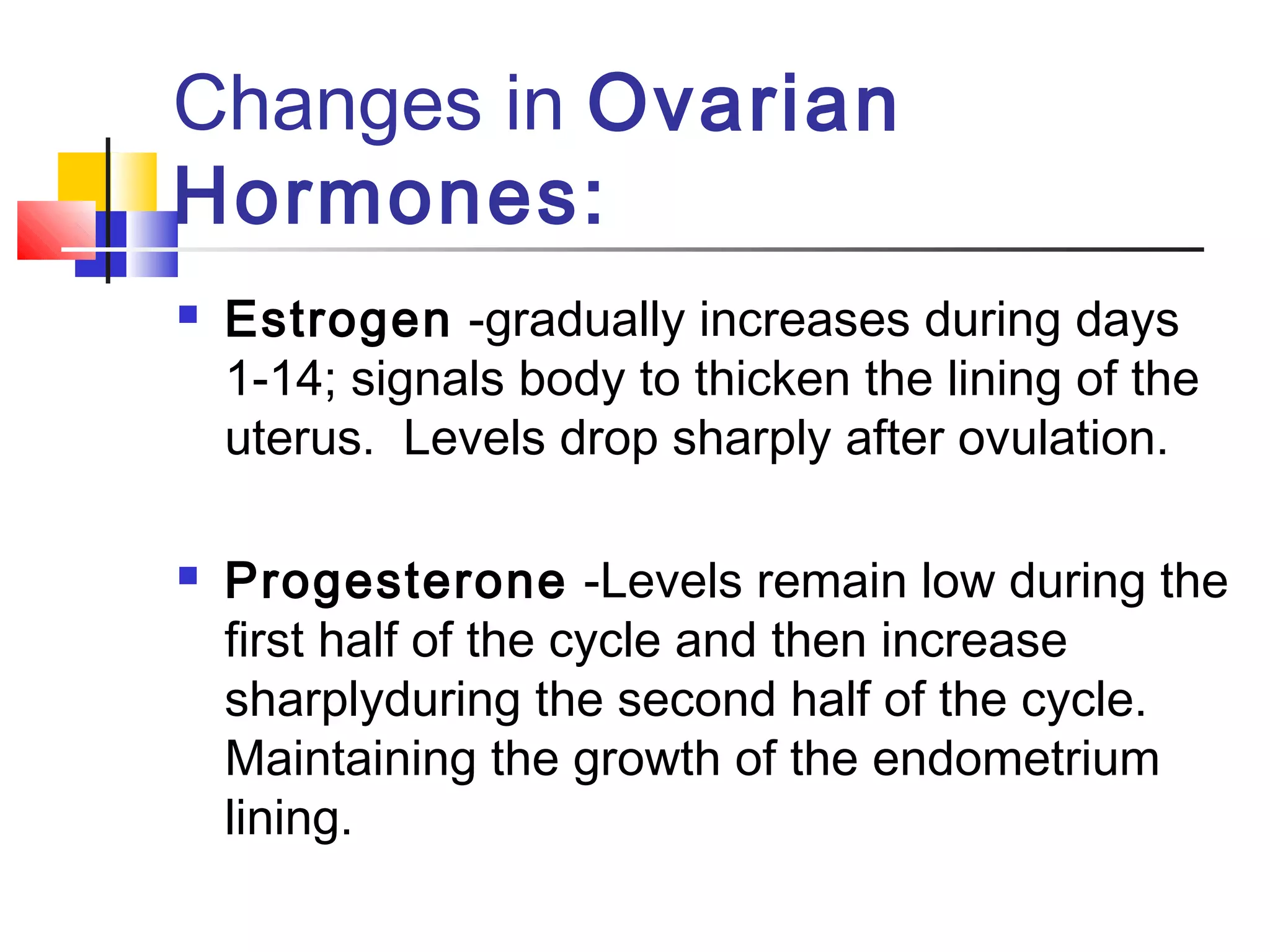
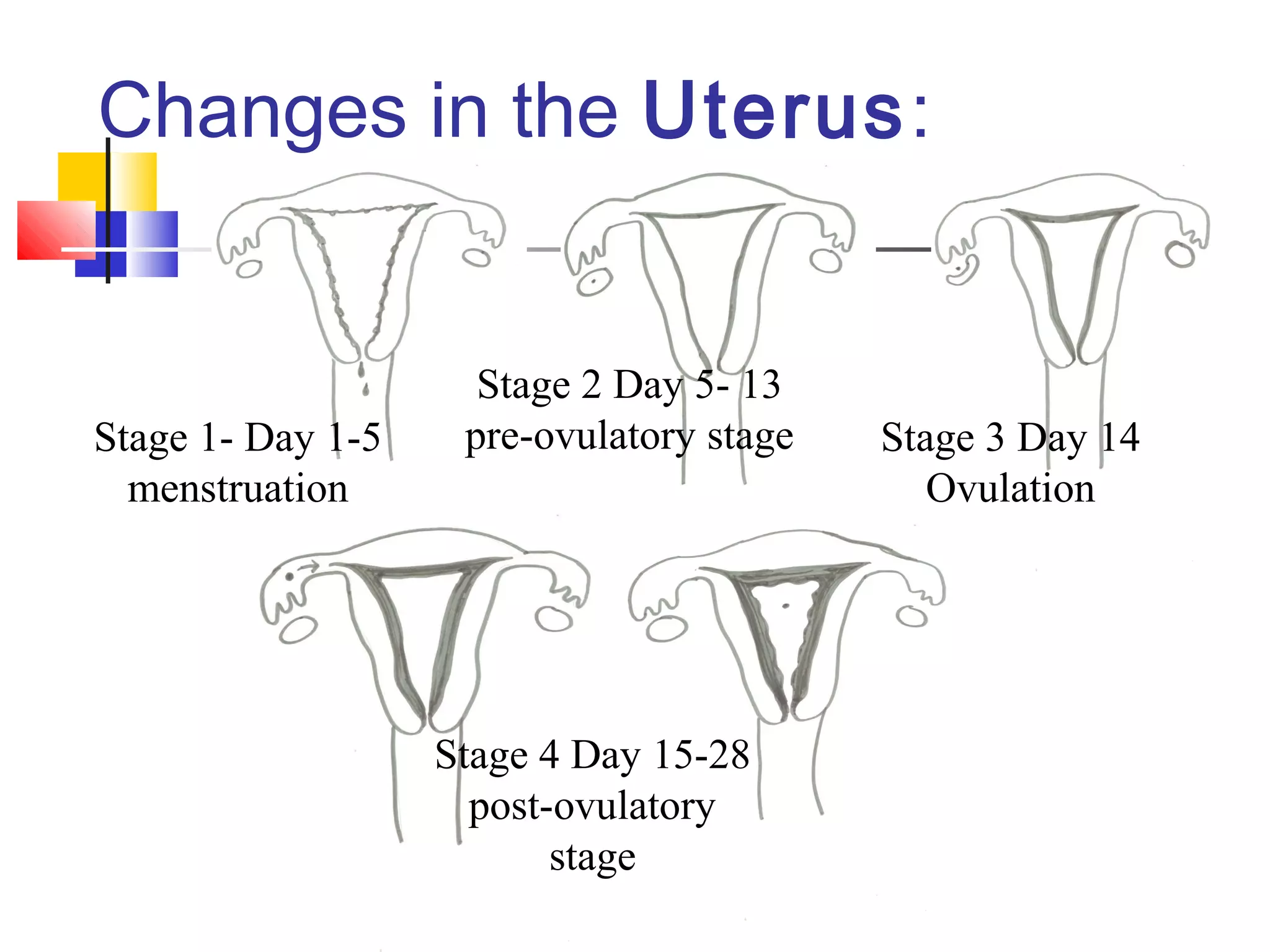
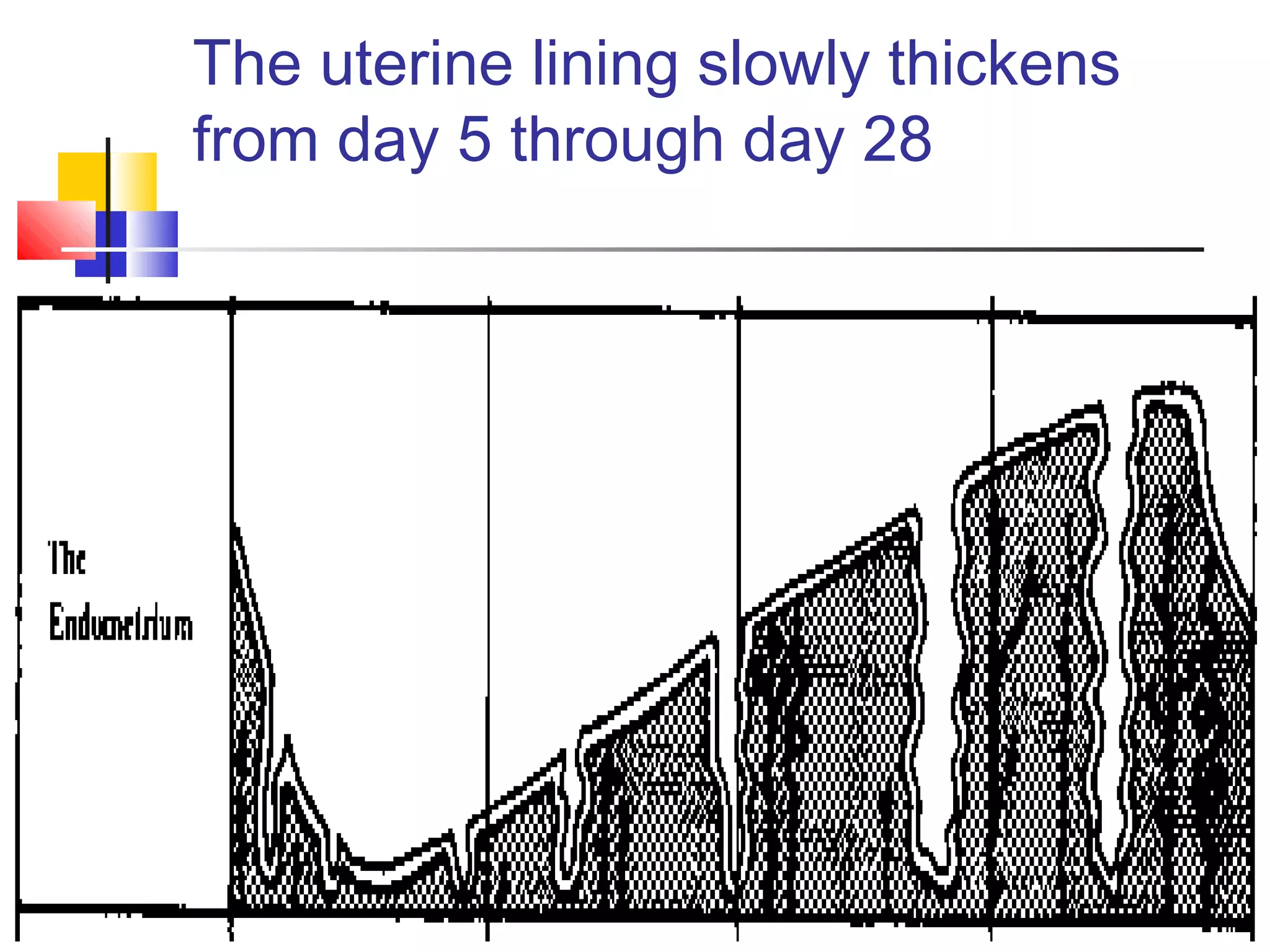
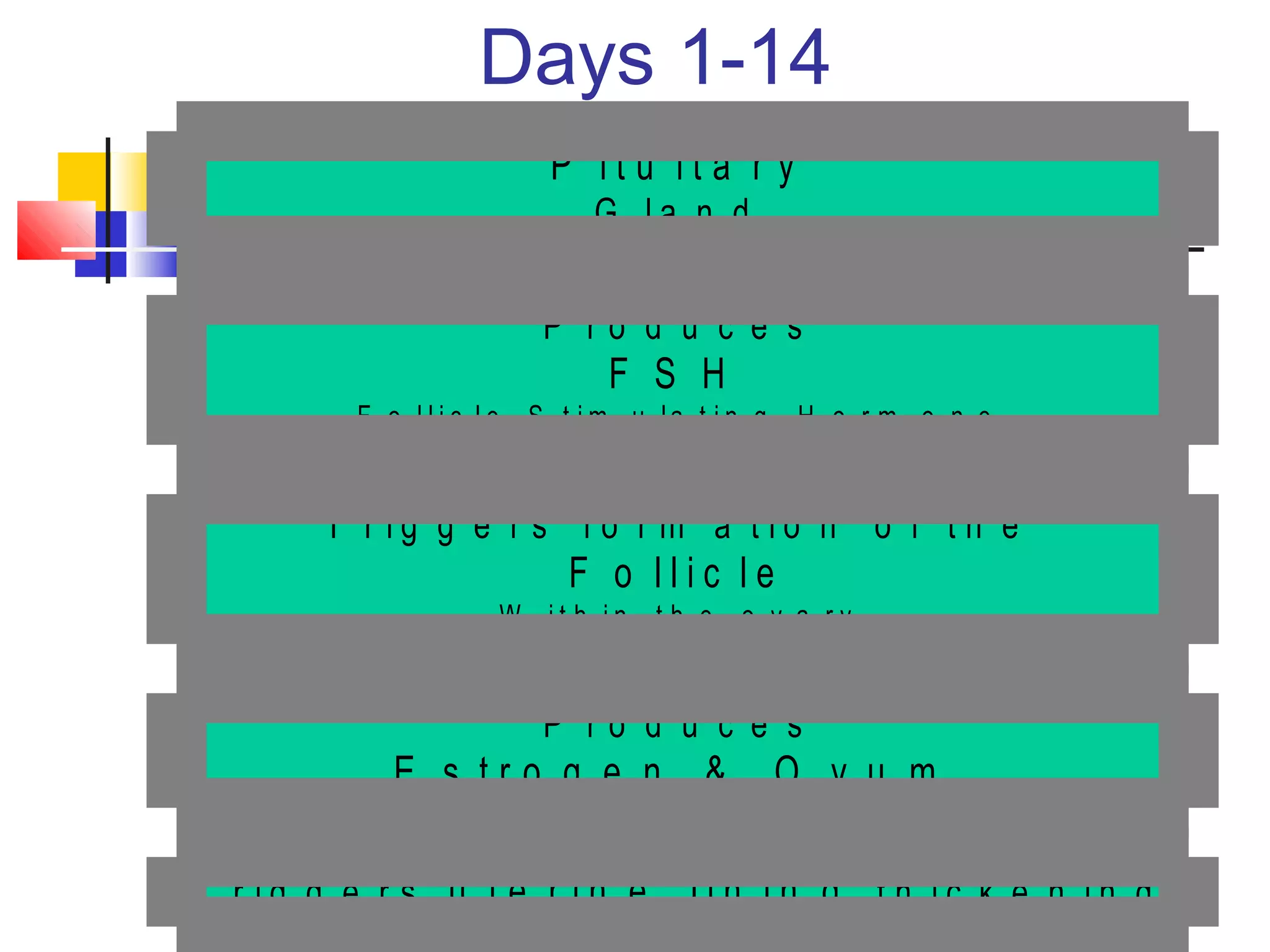
The menstrual cycle involves changes in the ovaries and uterus across approximately 28 days. In the first half, the pituitary gland releases FSH, stimulating egg maturation and estrogen production. Around day 14, LH triggers ovulation. If fertilization does not occur, progesterone and estrogen levels fall, causing the uterine lining to shed through menstruation and preparing the body for a new cycle. Precise hormonal interplay between the ovaries, pituitary gland, and uterus enables female reproduction.