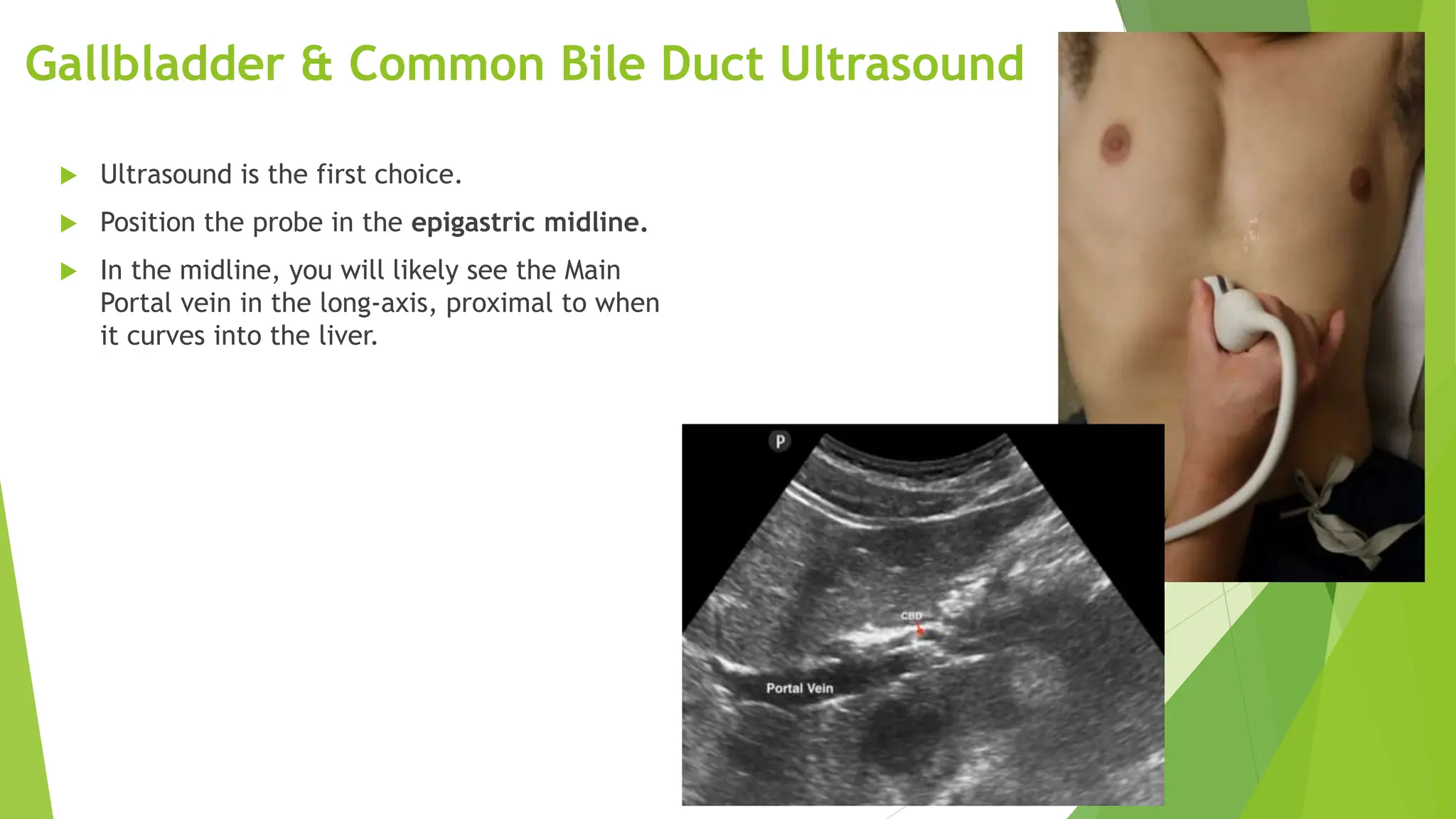
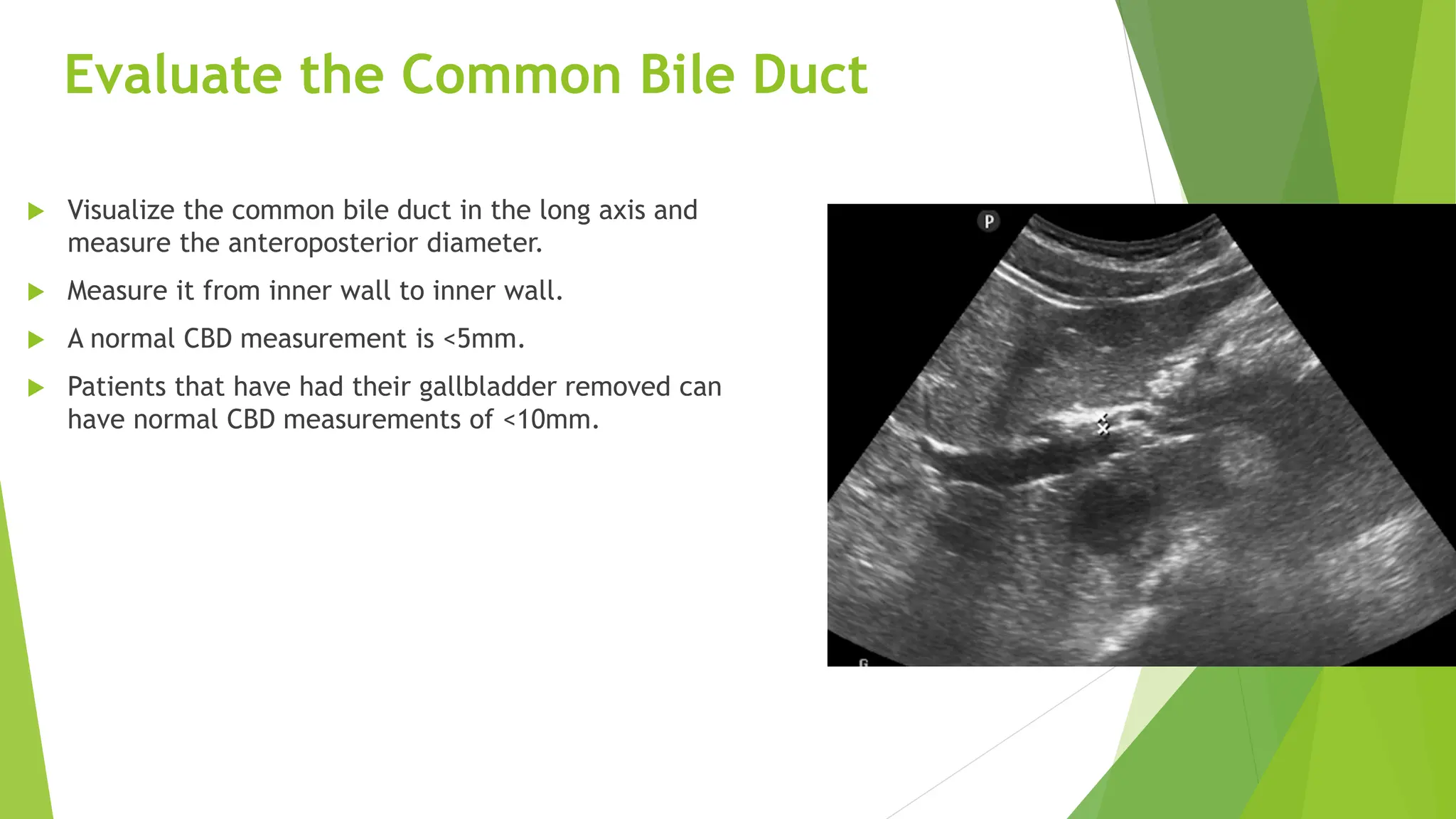
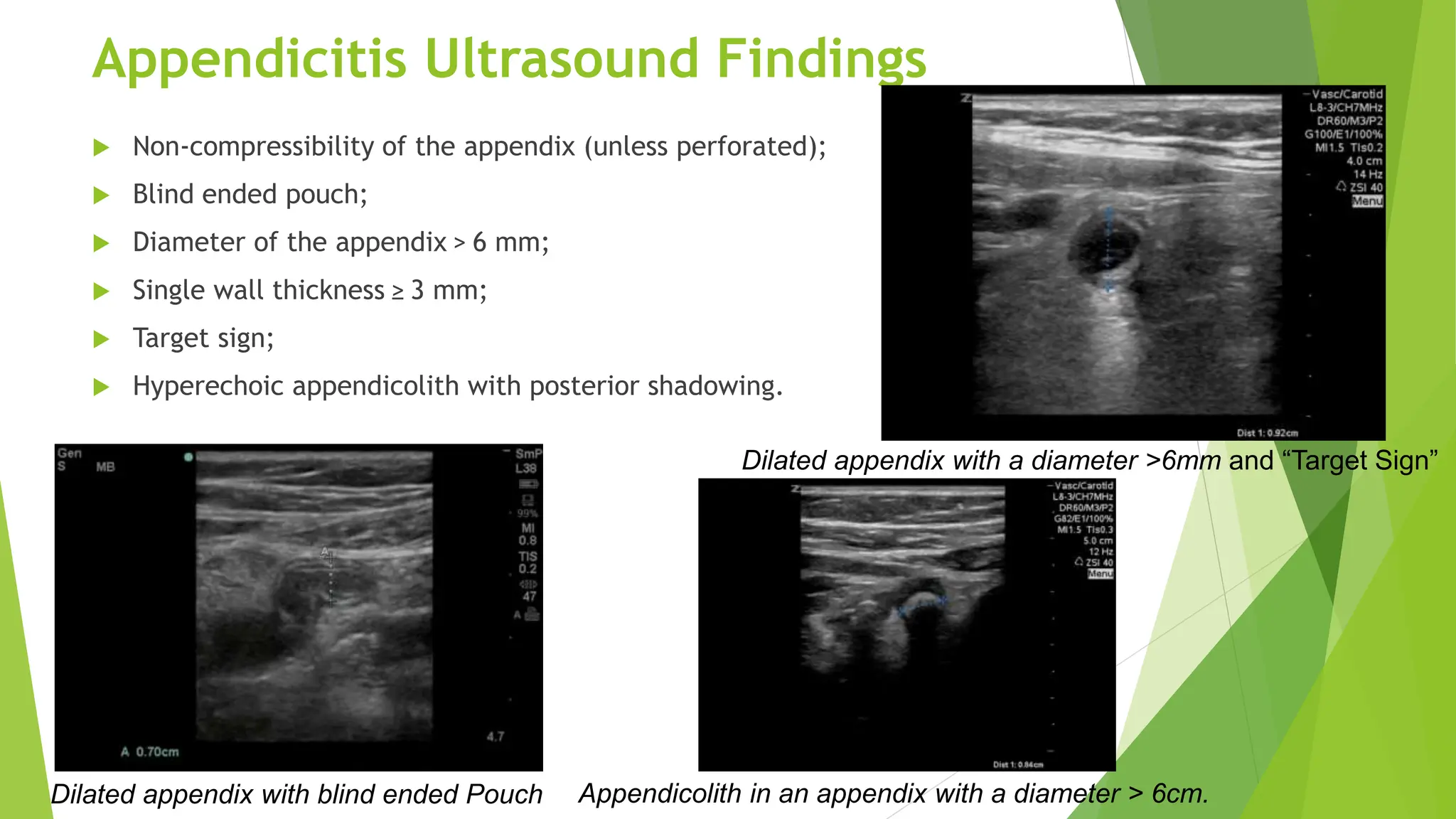
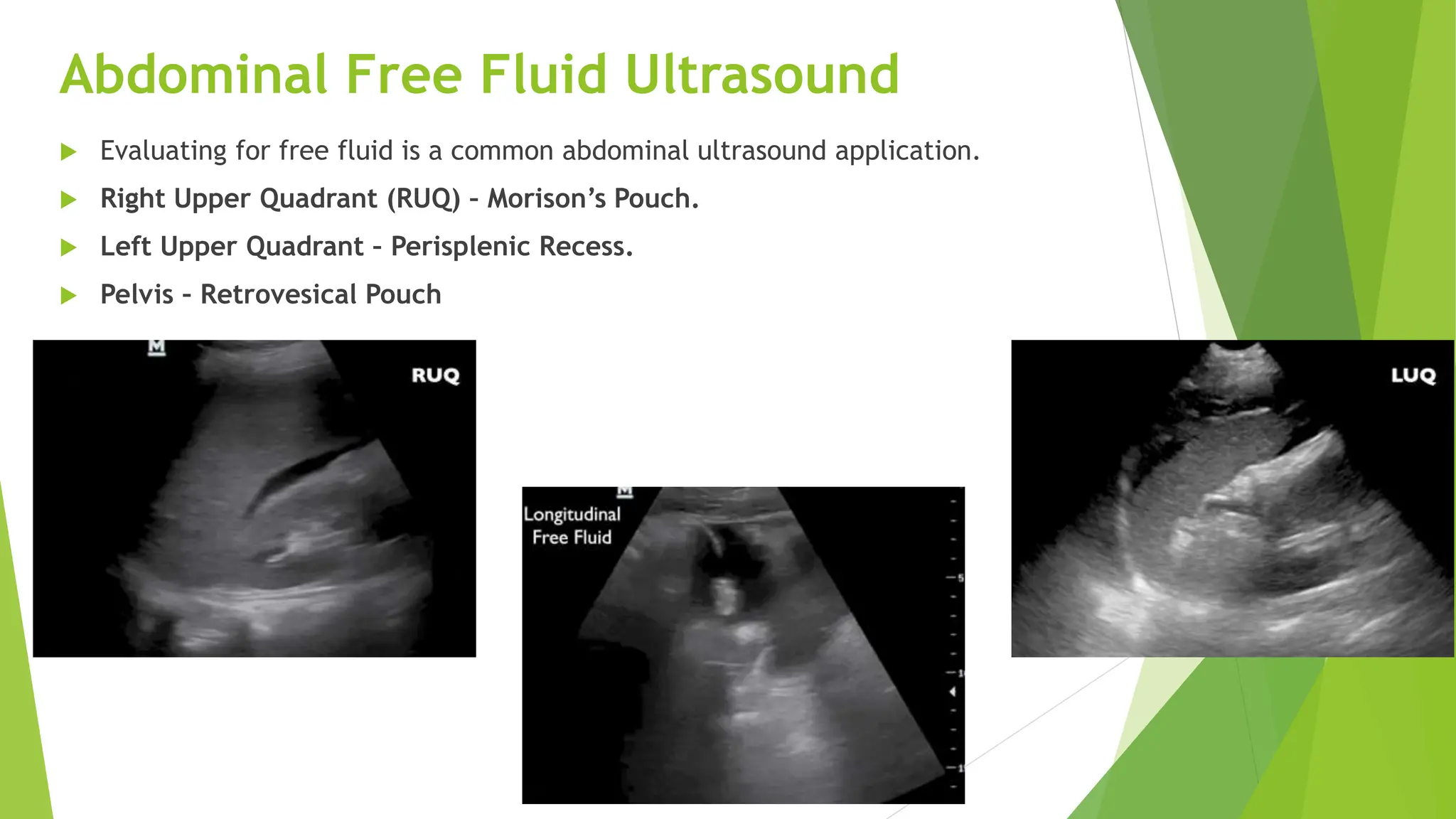
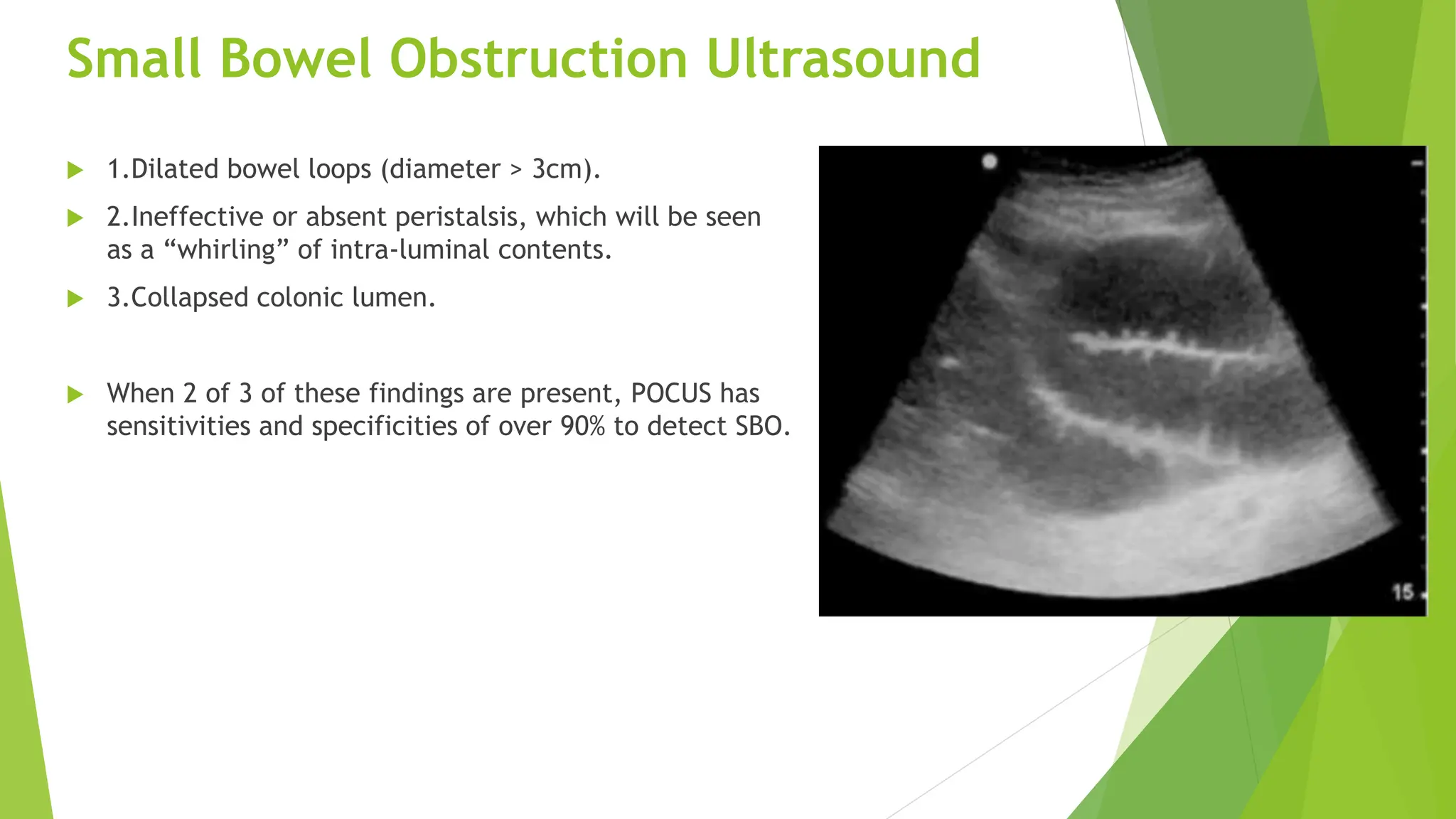
POCUS can rapidly and effectively evaluate many causes of abdominal pain. It can identify liver abnormalities like hepatitis or cirrhosis. The gallbladder and common bile duct can be examined for issues like cholecystitis or gallstones. Appendicitis is detectable by viewing an enlarged, non-compressible appendix. Small bowel obstructions appear as dilated bowel loops with reduced peristalsis. Free fluid and pneumoperitoneum can indicate internal bleeding or perforation. POCUS is a valuable tool for emergency evaluation of abdominal pain.