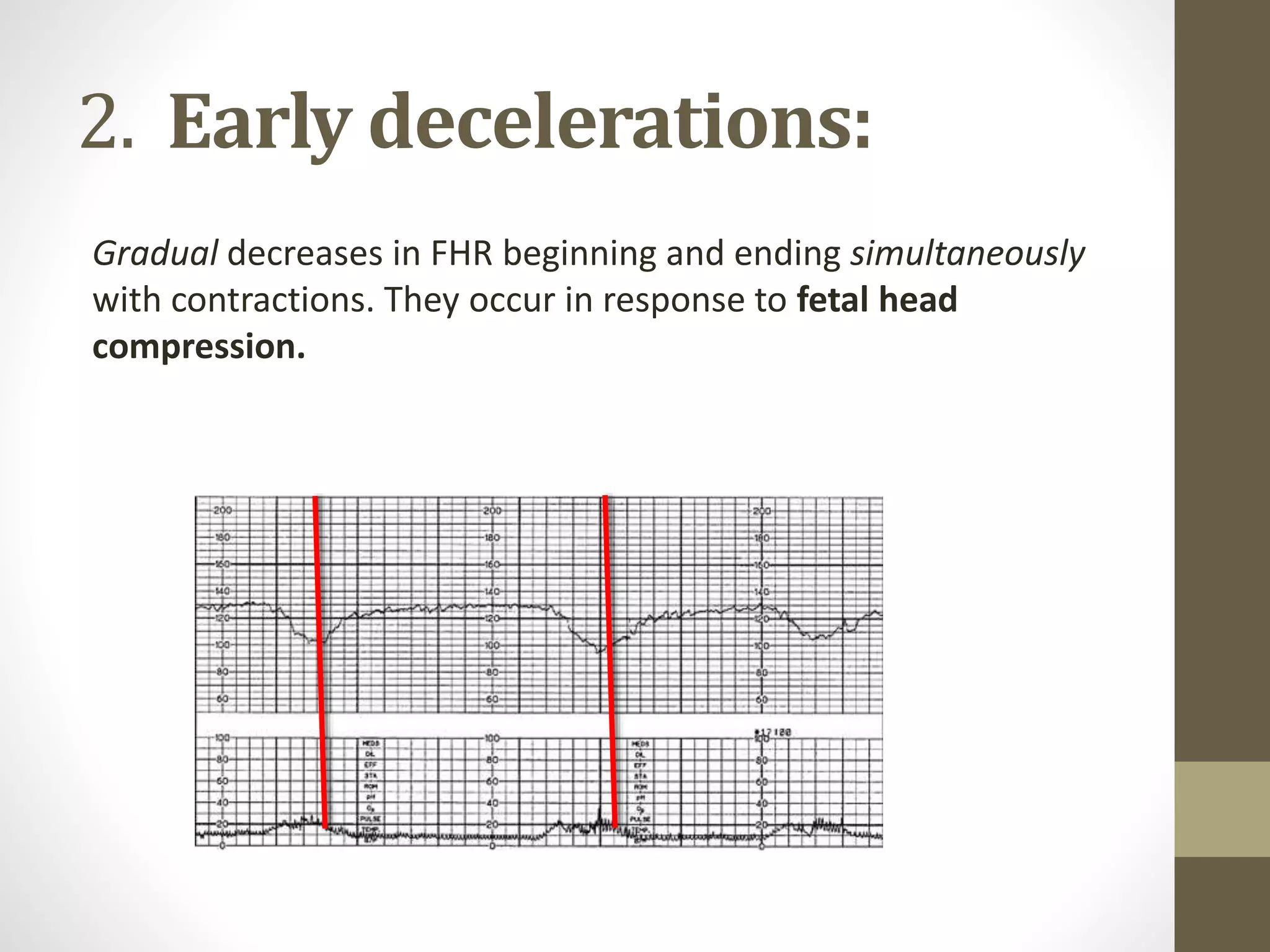
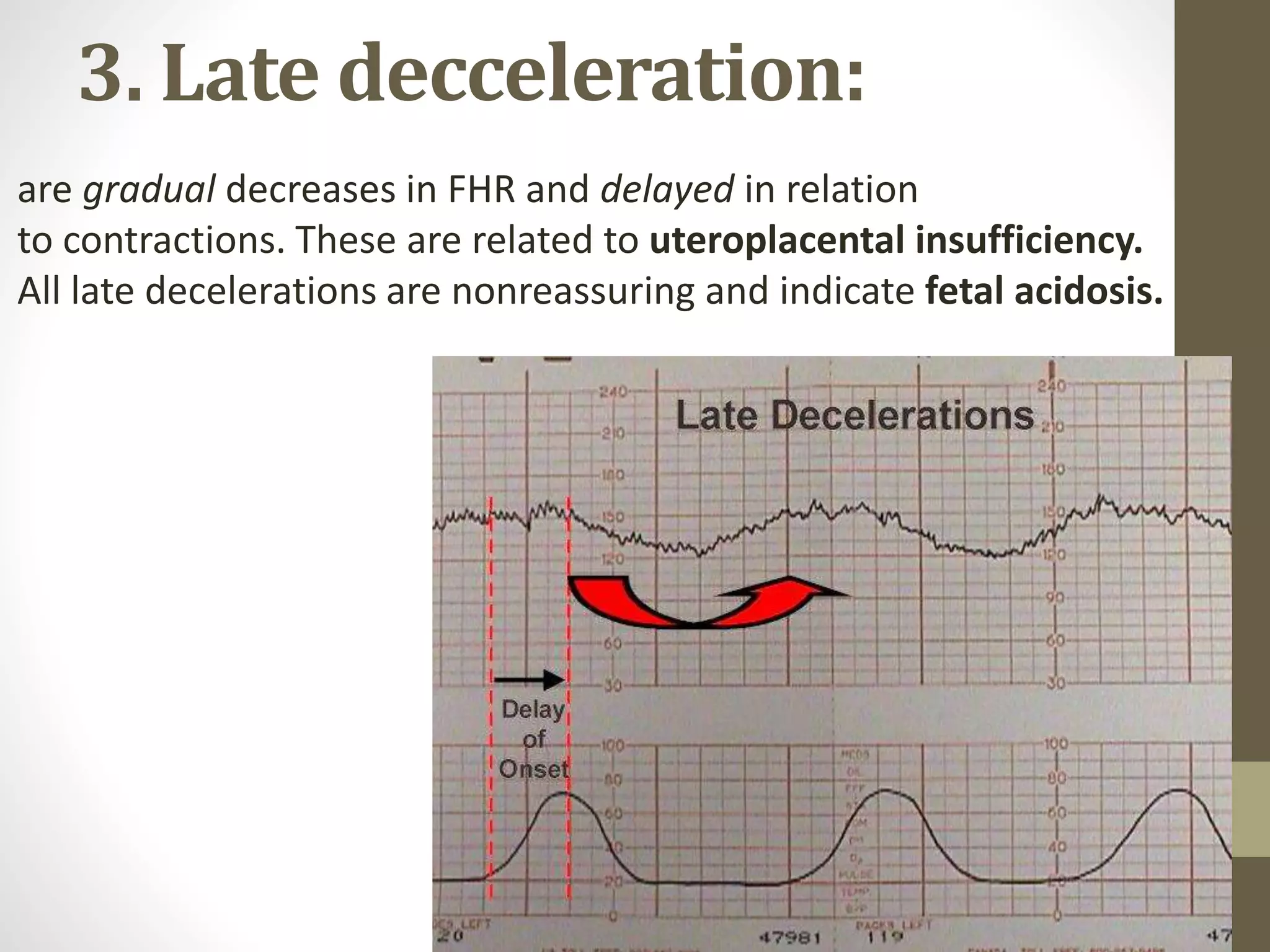
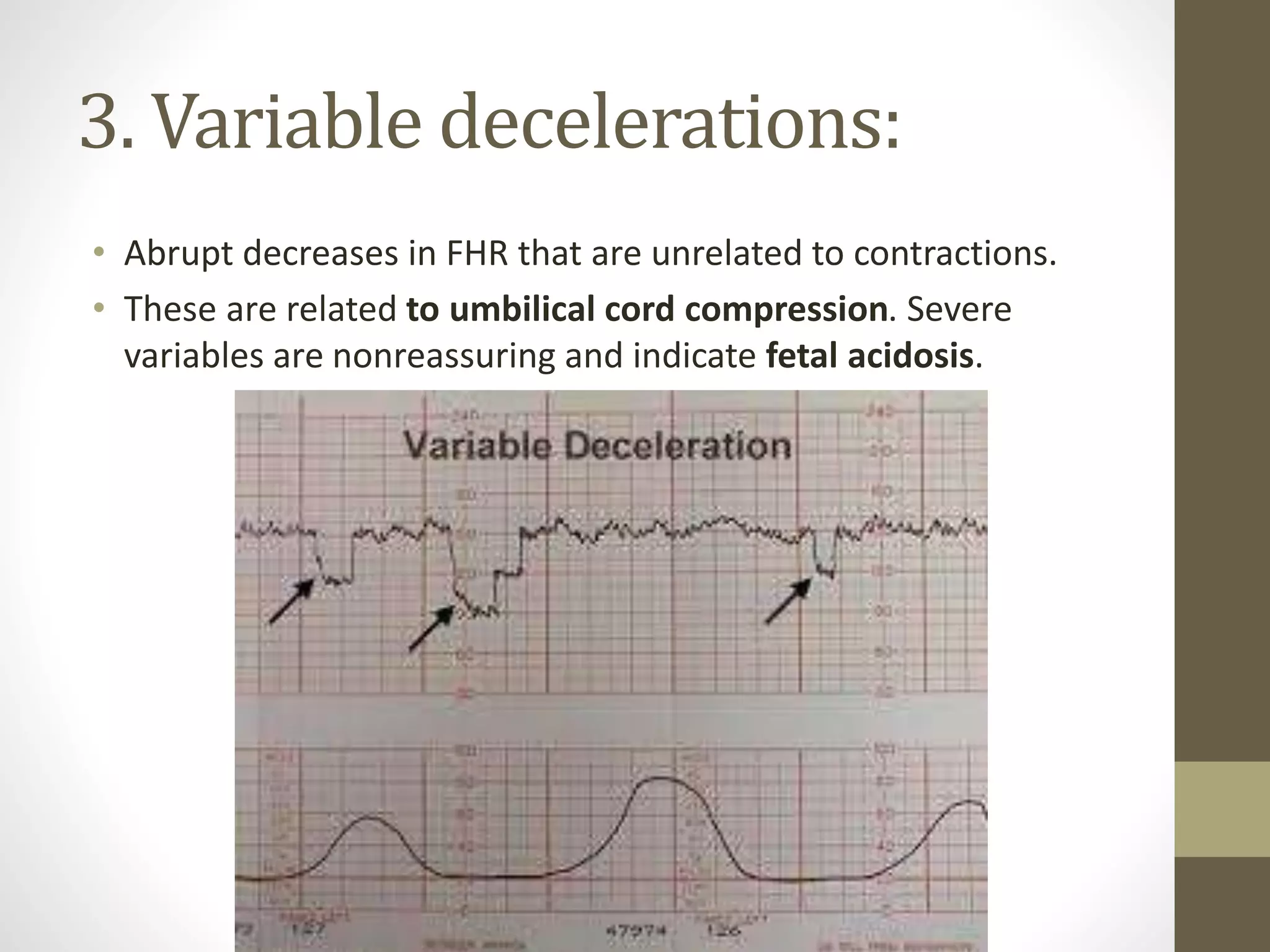
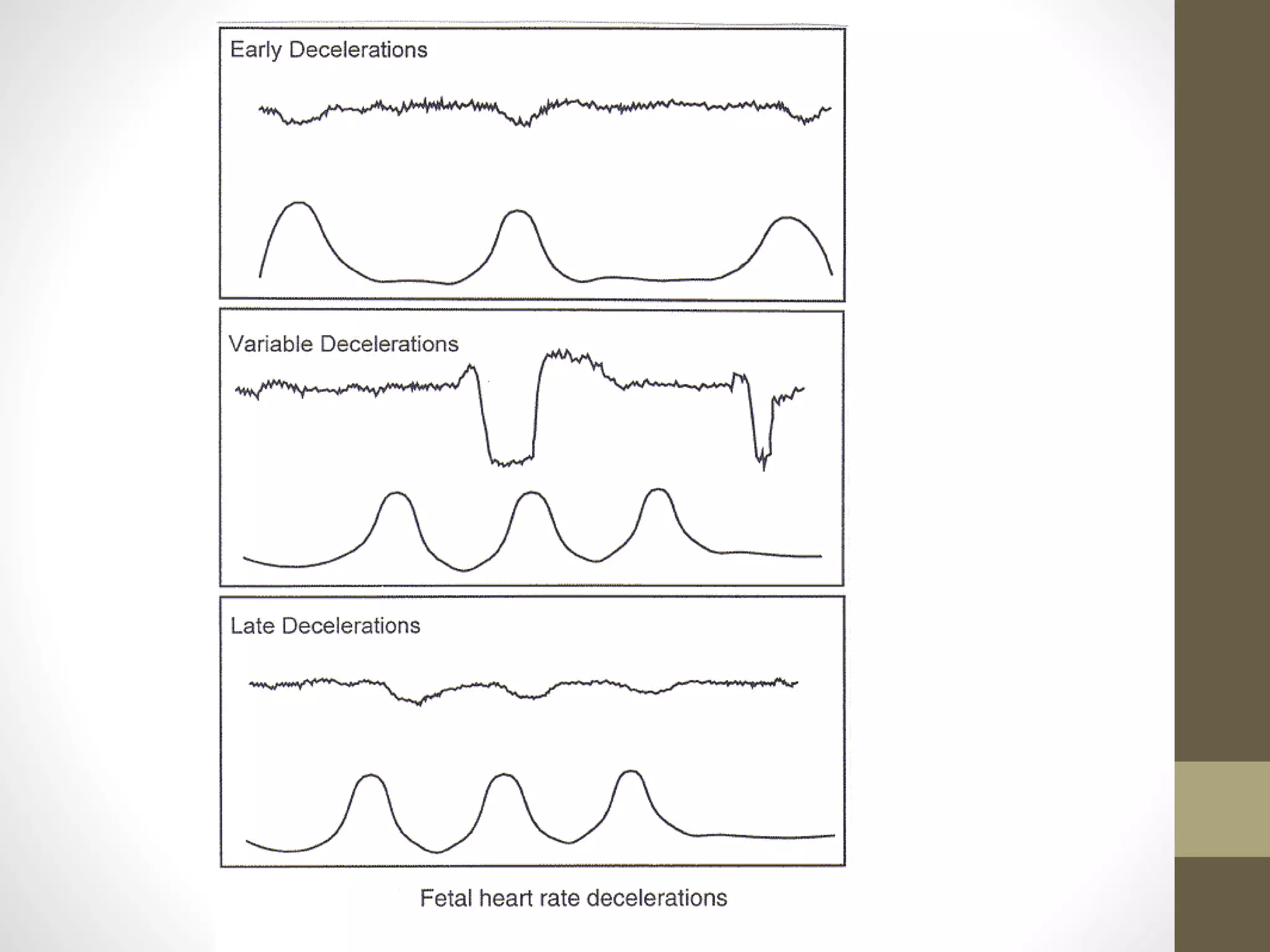
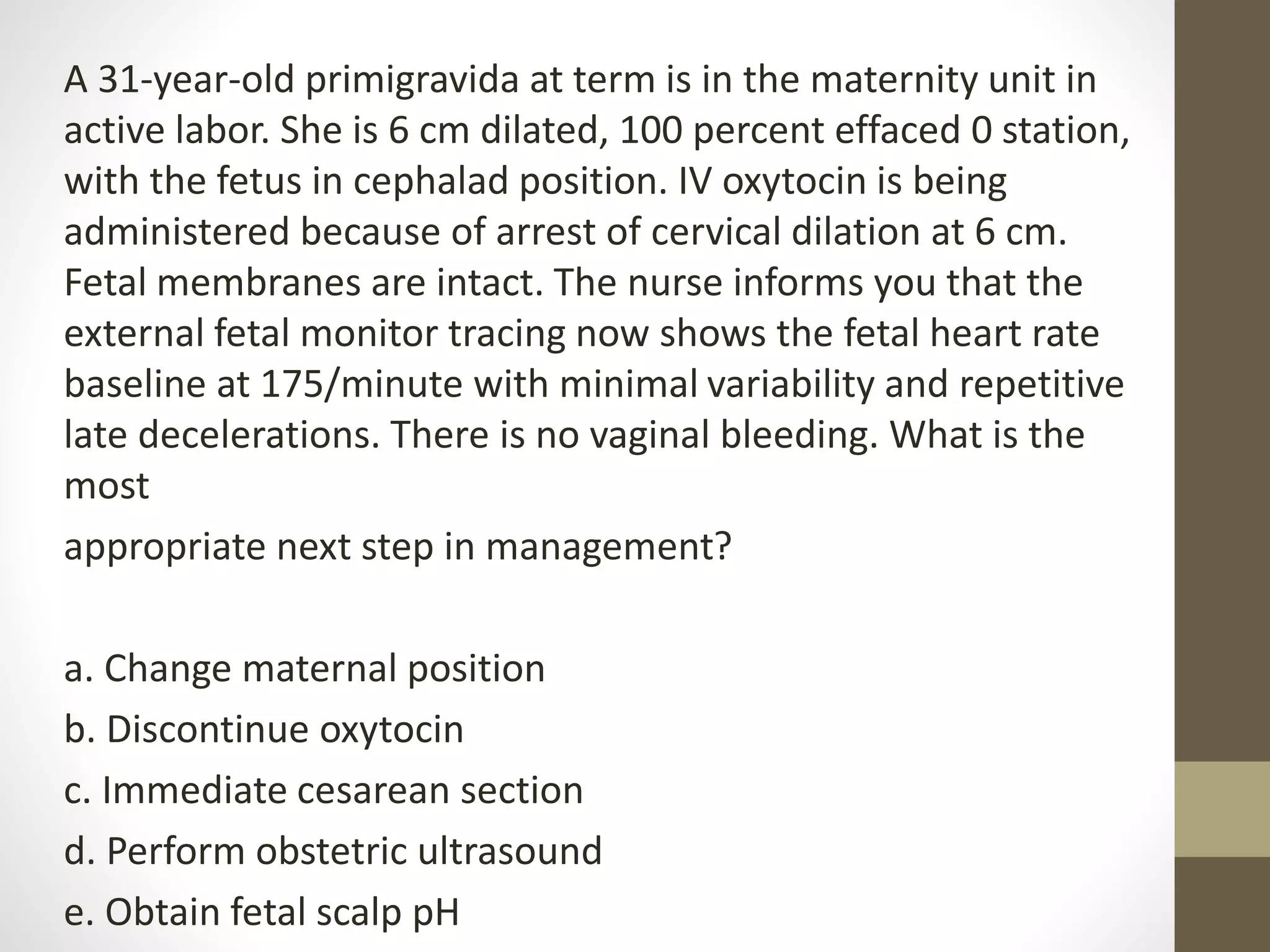
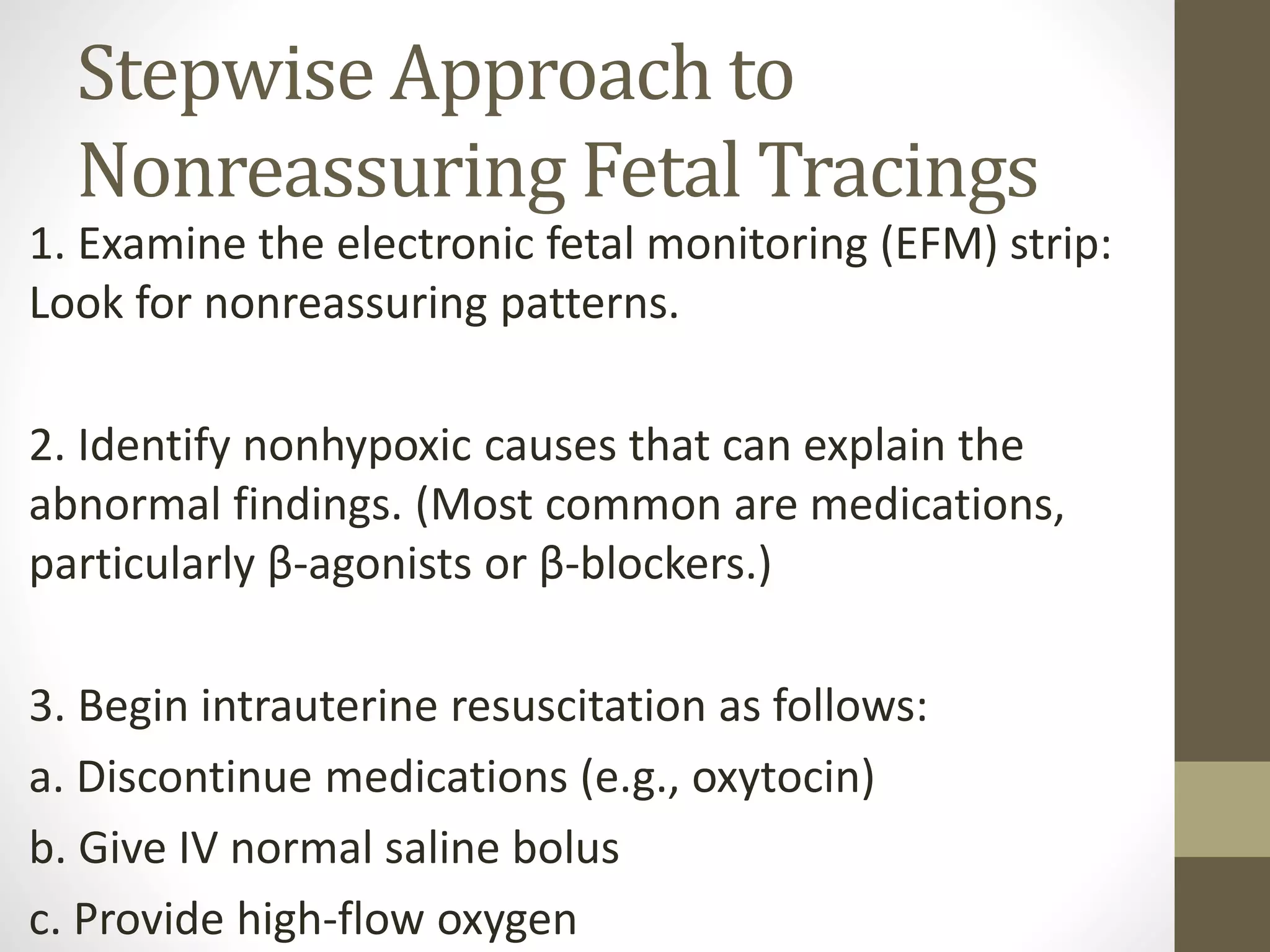
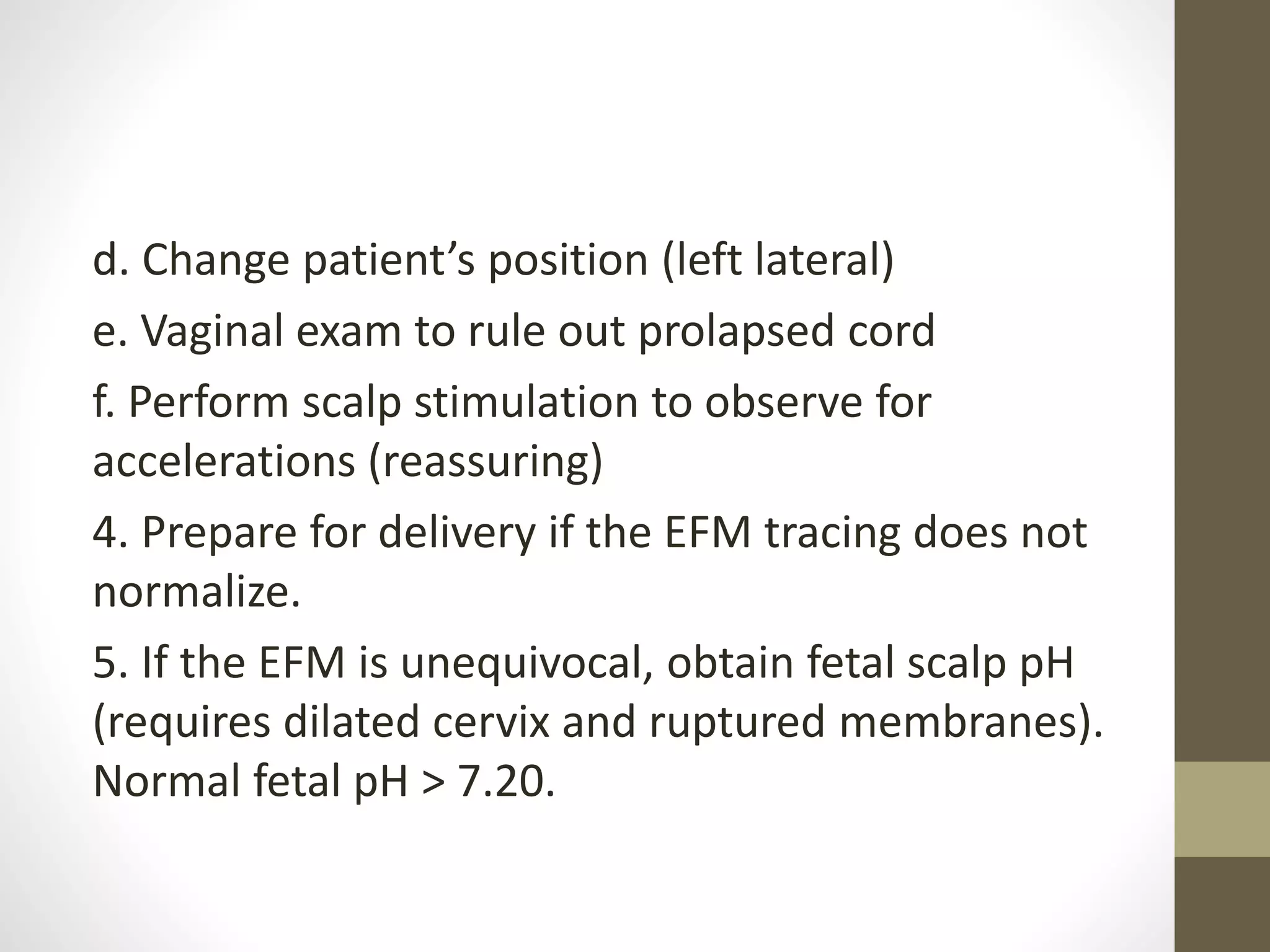
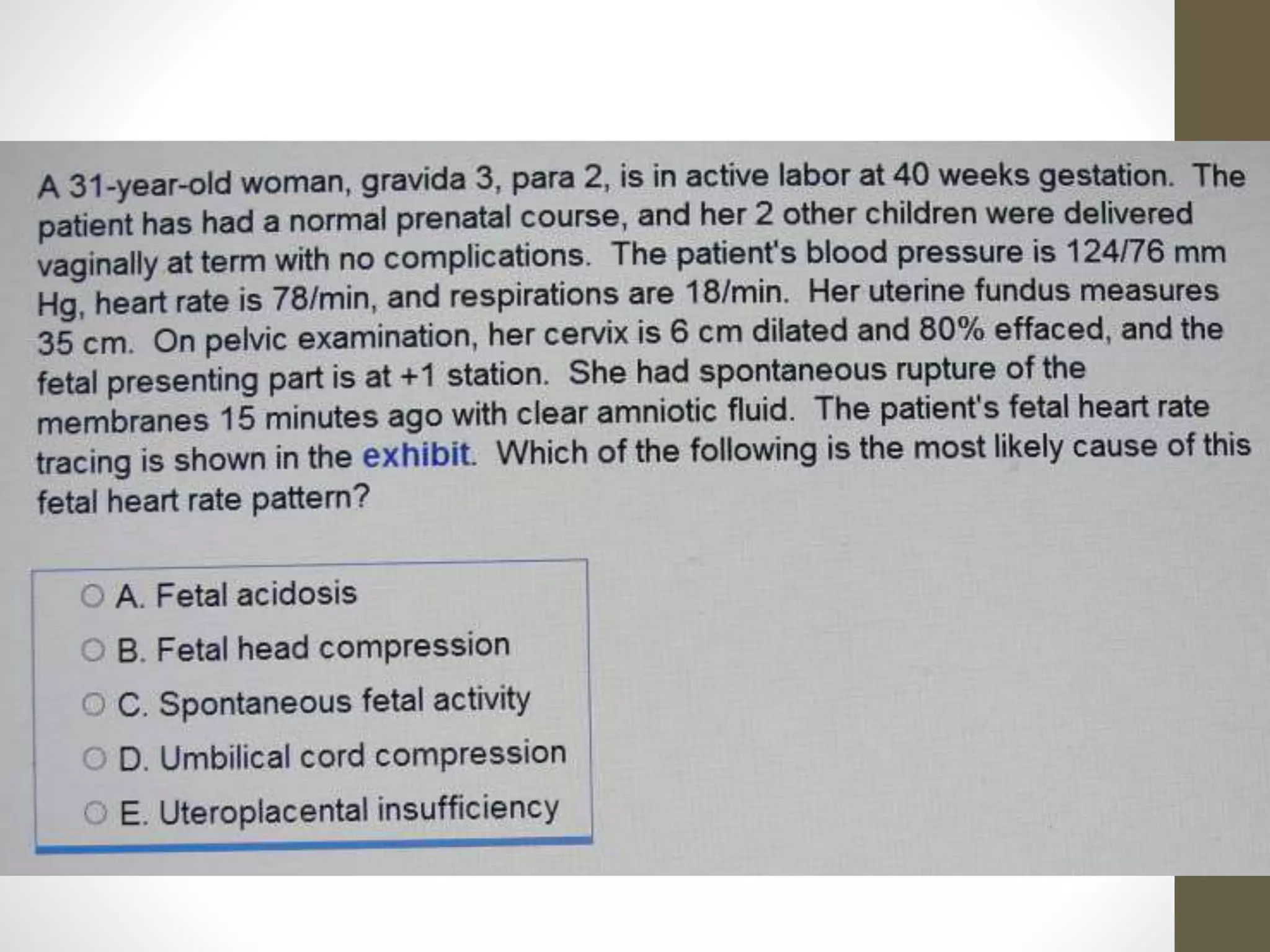
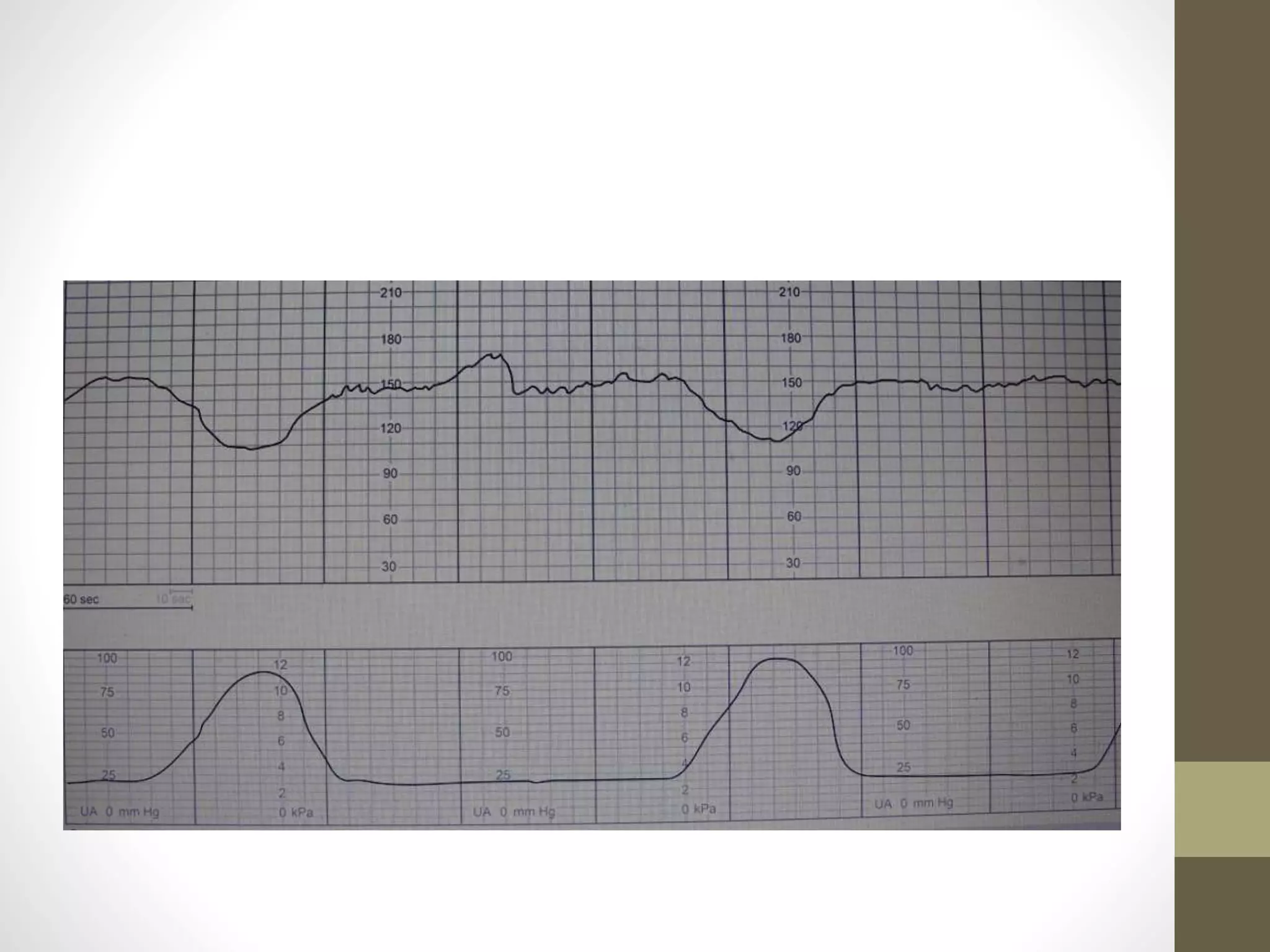
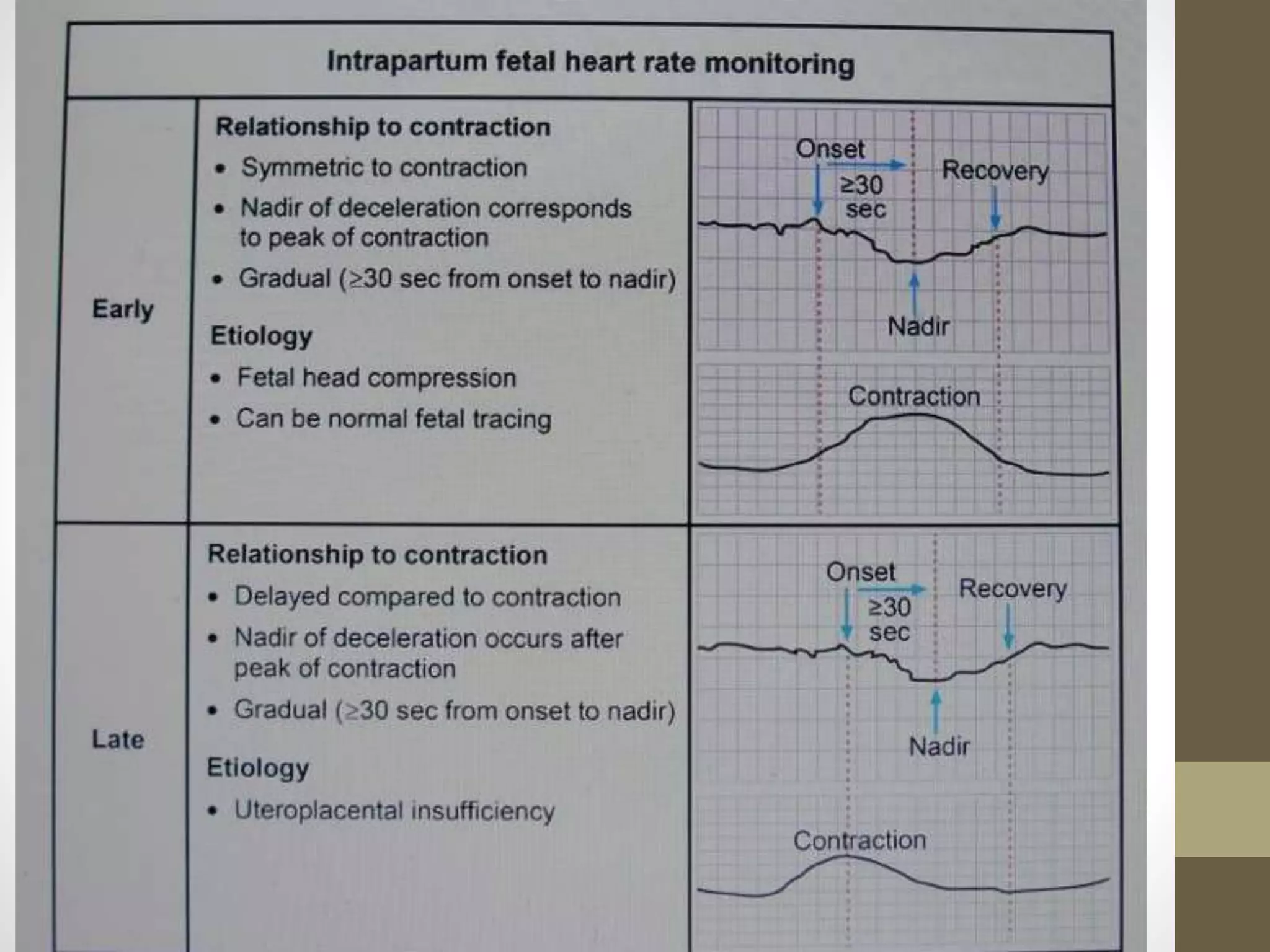
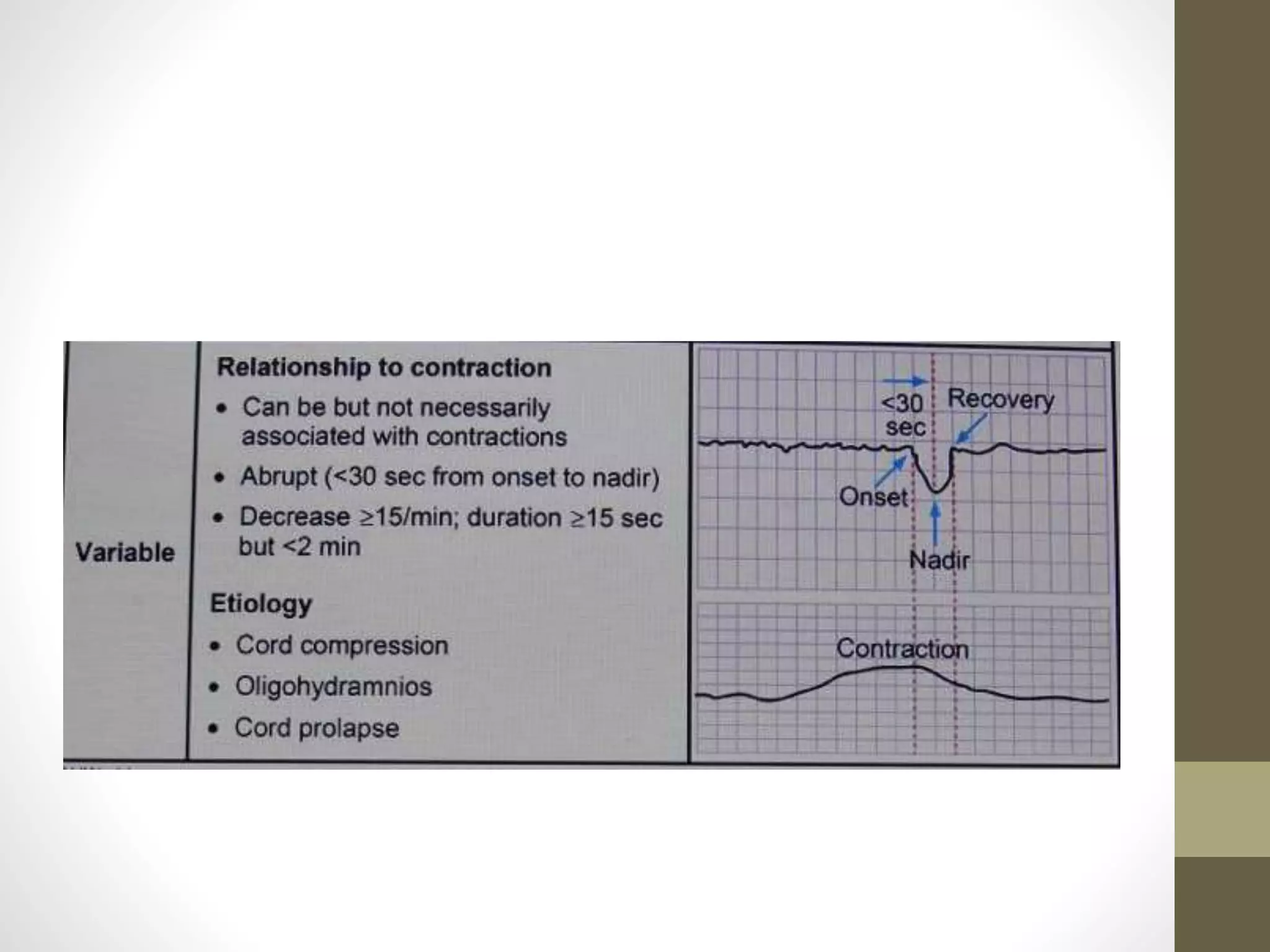
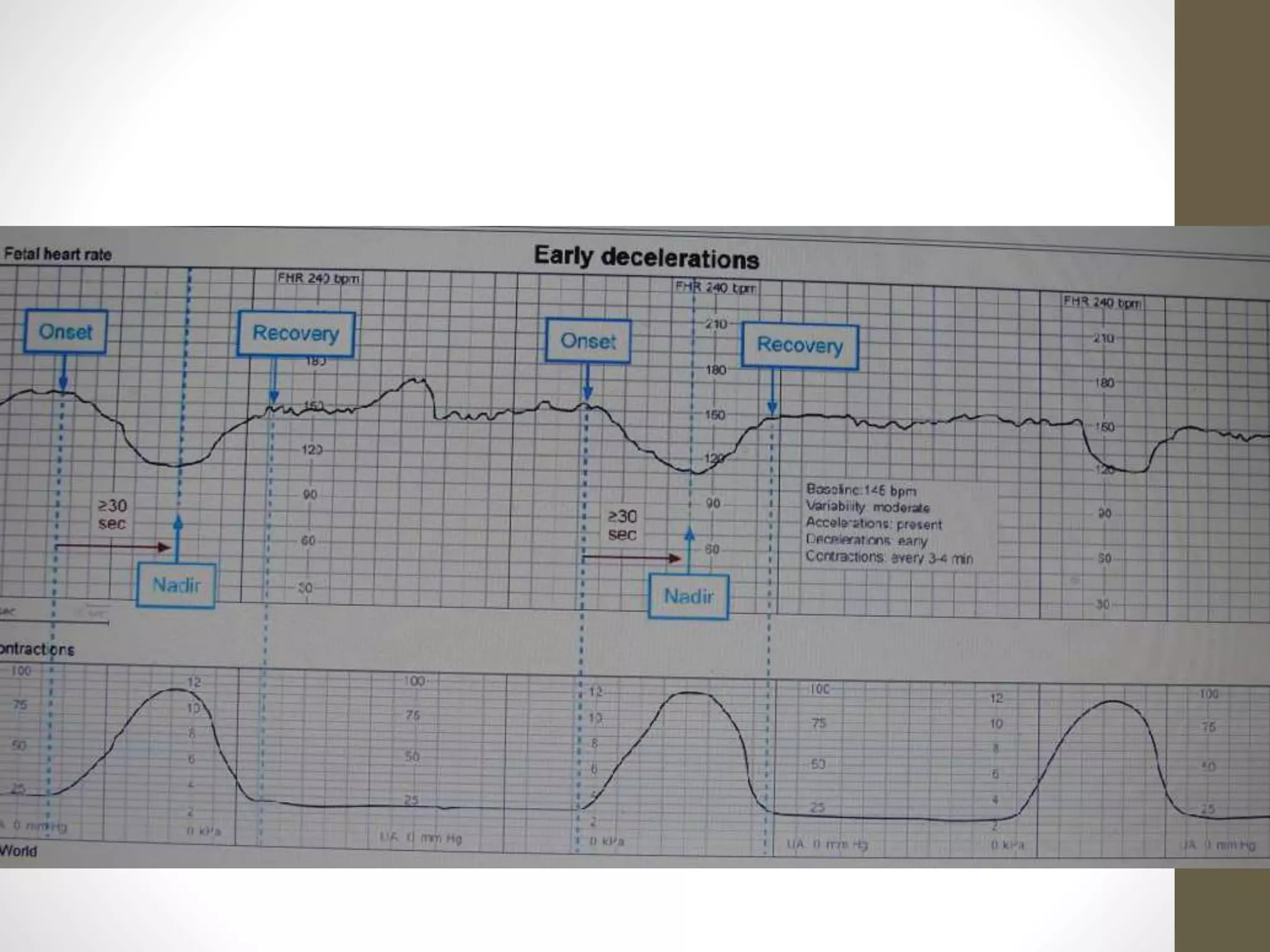
This document discusses evaluating fetal heart tracings by assessing the baseline heart rate, periodic changes, and decelerations. It provides details on normal ranges and causes of abnormalities. When presented with a case of a patient in active labor with minimal heart rate variability and repetitive late decelerations, the recommended next step is to discontinue oxytocin administration, as medications are a common cause of nonreassuring tracings. A stepwise approach to management is then outlined.