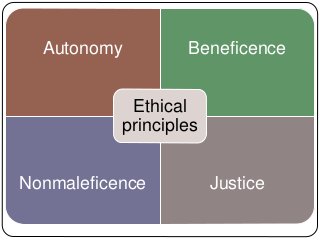
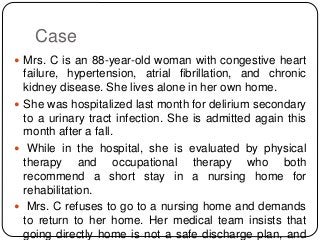
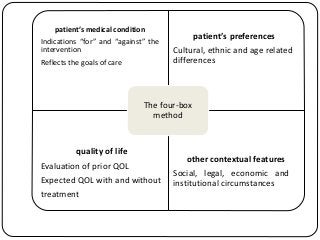
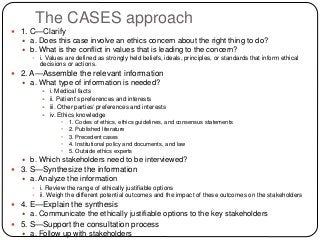
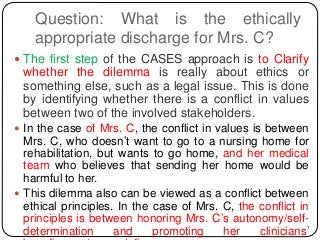
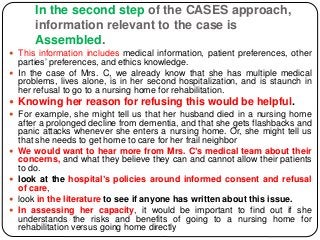
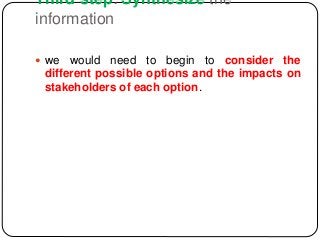
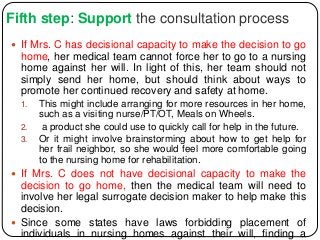
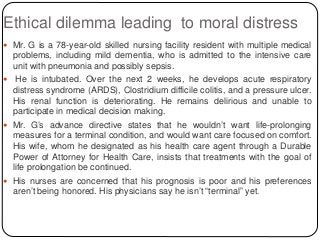
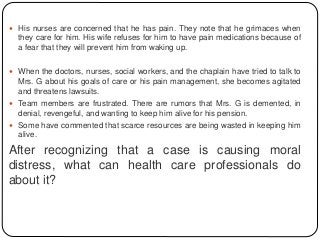
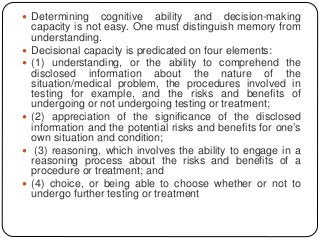
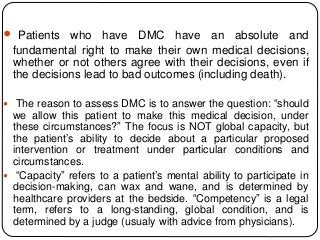
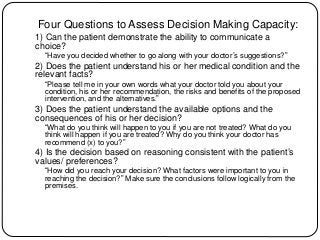
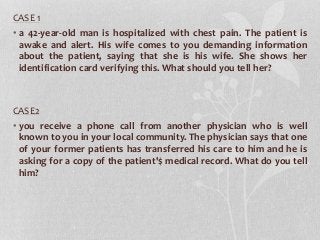
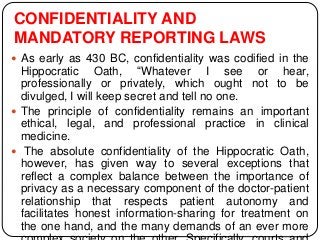
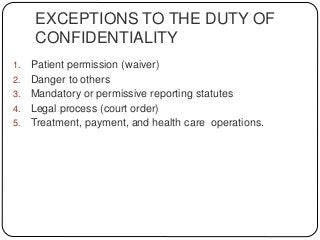
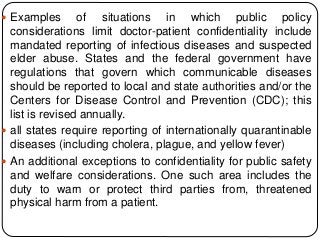
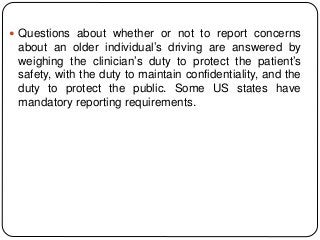
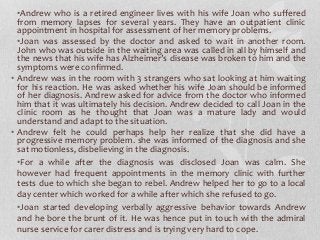
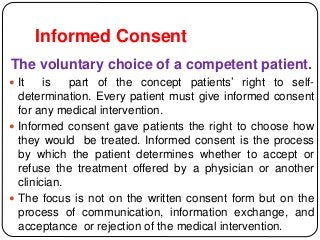
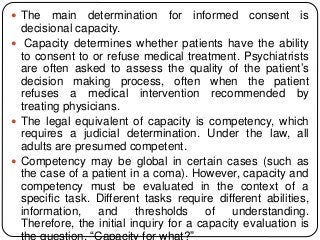
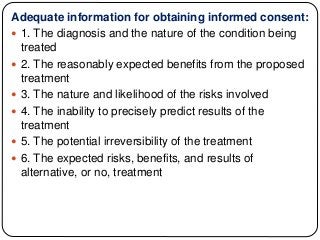
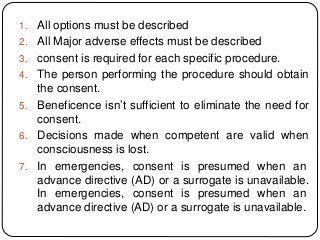
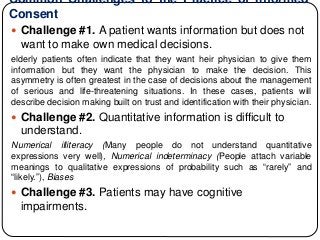
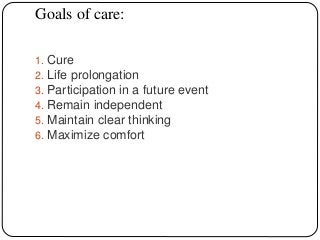
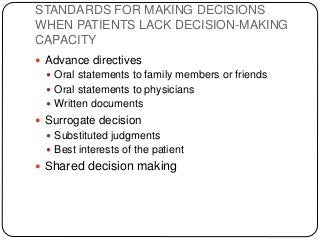
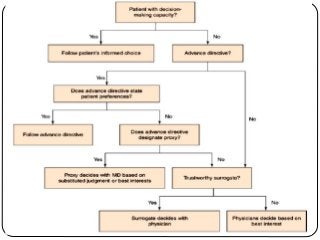
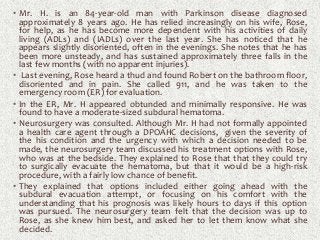
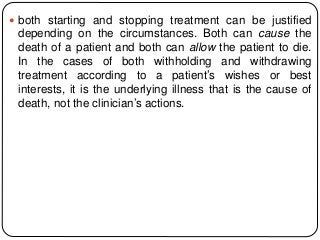
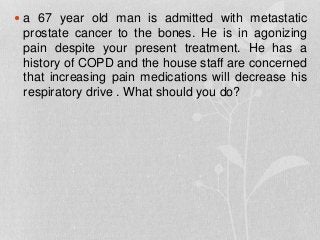
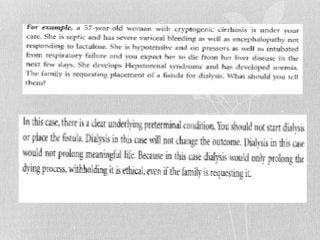
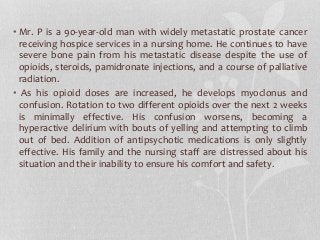
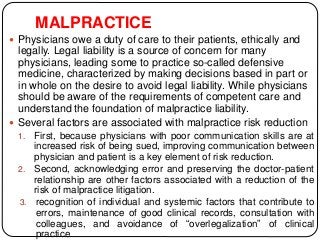
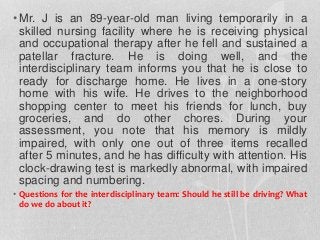
The document summarizes key ethical issues in geriatric care including principles of autonomy, beneficence, and nonmaleficence. It discusses approaches to analyzing ethical dilemmas, including the four-box method and CASES framework. It also covers topics like moral distress, assessing decision-making capacity, and confidentiality/mandatory reporting laws. Specifically, it provides a case example of an elderly patient refusing discharge to a nursing home and walks through applying the CASES approach to determine the ethically appropriate discharge plan.

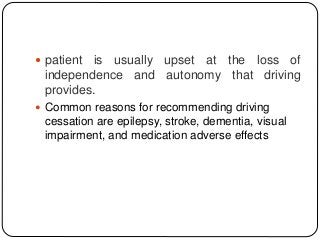
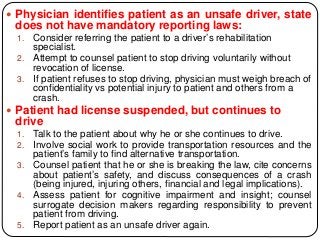
![STRATEGIES TO EMPLOY WHEN WORKING WITH OLDER
ADULTS REGARDING DRIVING CESSATION
Patient threatens to sue physician if reported to
Department of Motor Vehicles:
1. Clearly document how the patient was determined to
be an unsafe driver (driving fitness evaluation,
assessing driving-related skills [ADReS] battery,
driving rehabilitation referral, medications, etc).
2. Advise patient that the state has the ultimate
responsibility to determine licensing.
3. If physician is mandated to report in that state,
physician must report. The physician should also
advise the patient of this.
4. Consult malpractice insurance or legal counsel to
determine degree of risk (physicians generally run](https://image.slidesharecdn.com/ethicalissues-181103224337/85/Ethical-issues-in-geriatric-care-119-320.jpg?cb=1676624462)