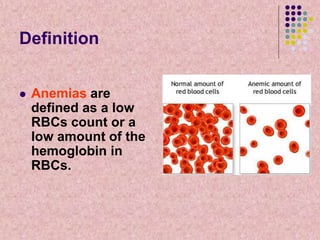
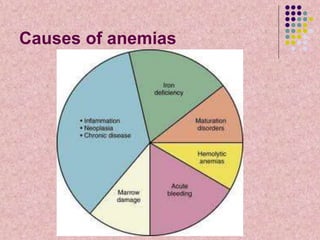
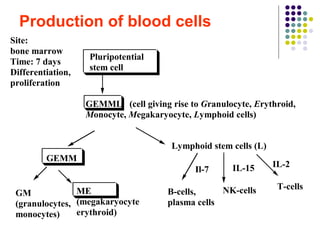
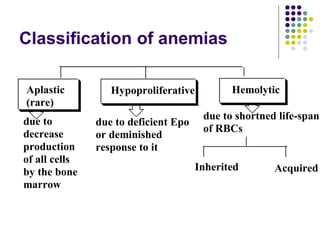
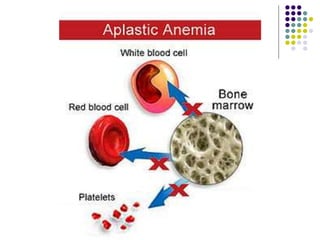
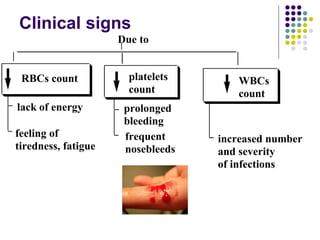
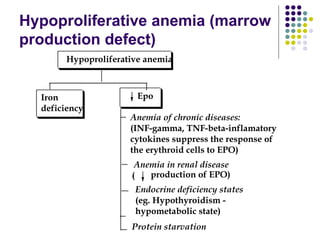
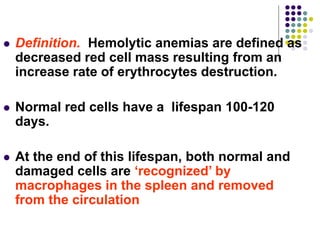
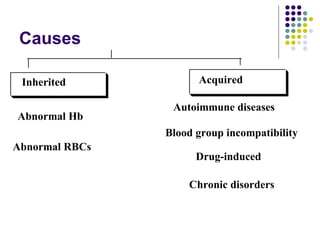
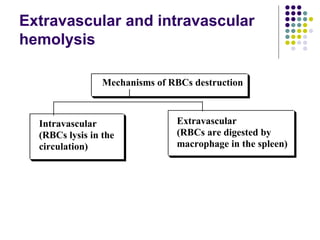
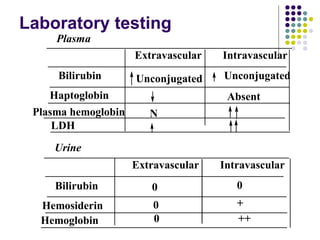
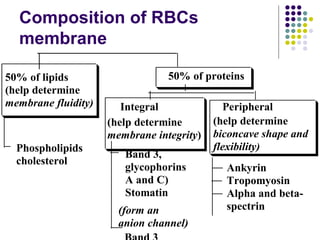
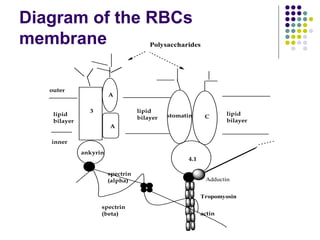
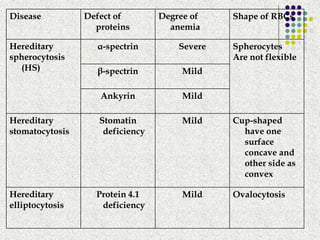
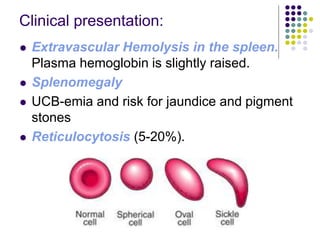
Anemias are caused by a low red blood cell (RBC) count or low hemoglobin in RBCs. There are three main types of anemia: hypoproliferative anemia caused by decreased RBC production; hemolytic anemia caused by increased RBC destruction; and aplastic anemia caused by rare damage to stem cells in the bone marrow. Hemolytic anemias specifically result from a shortened RBC lifespan, where the bone marrow cannot replace destroyed RBCs quickly enough. Membrane defects can also cause hemolytic anemia, such as hereditary spherocytosis caused by alpha or beta spectrin deficiencies, which results in spherical RBCs more vulnerable to spleen destruction.