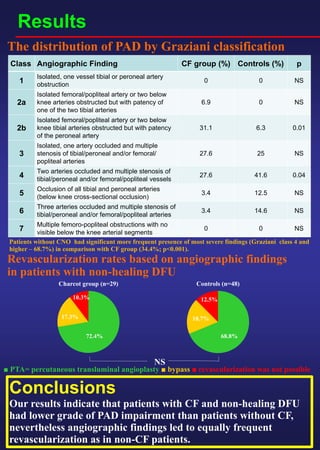
This document compares angiographic findings between patients with non-healing diabetic foot ulcers (DFUs) with and without Charcot foot (CF). It found that patients with CF and DFUs had less severe peripheral arterial disease (PAD) based on angiographic findings compared to DFU patients without CF, however revascularization rates were equal between the two groups. The study assessed 29 CF patients and 48 non-CF patients with DFUs who underwent lower limb angiography. It found patients without CF had significantly more frequent presence of severe PAD (Graziani class 4 and higher) versus the CF group.