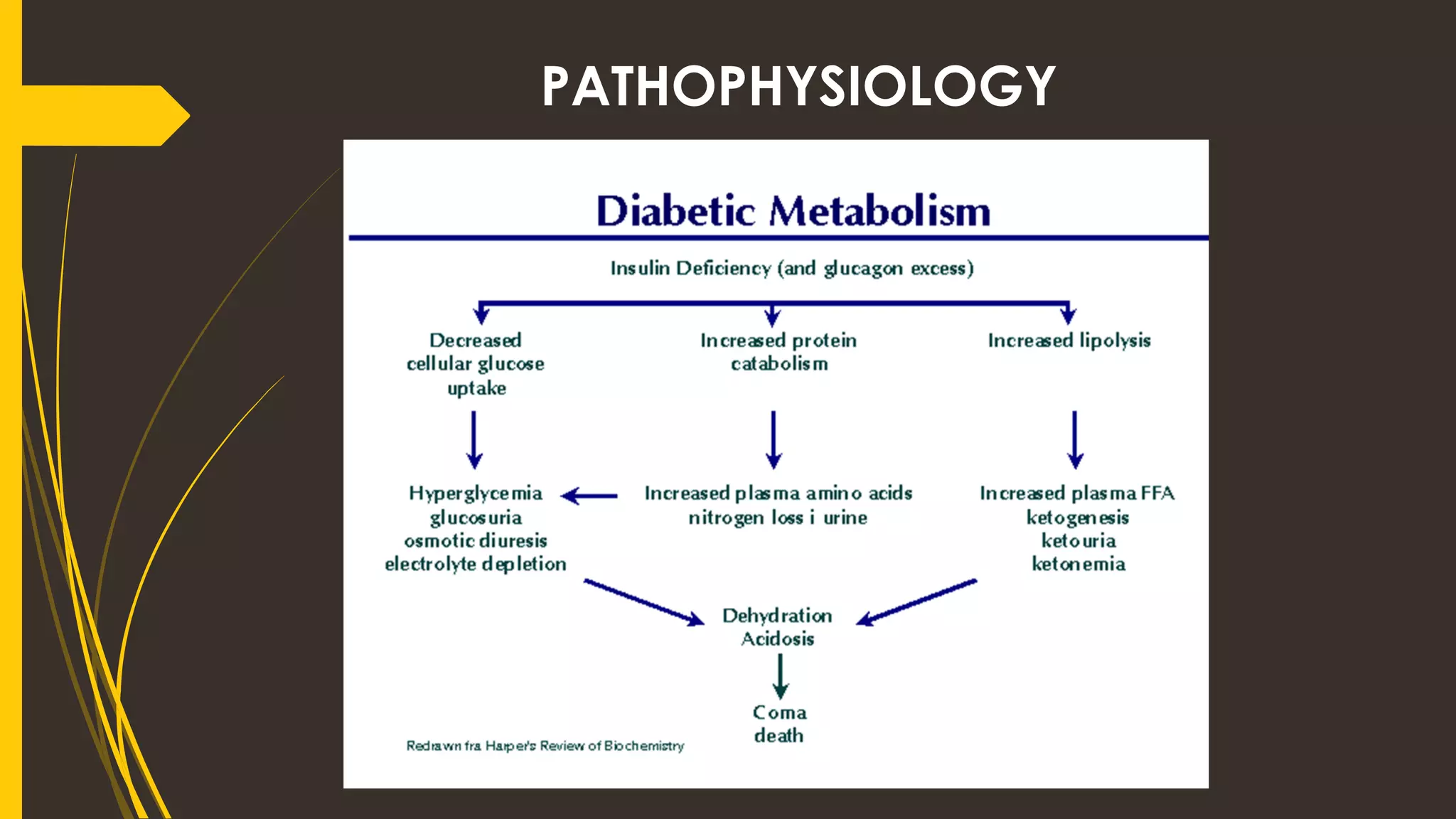
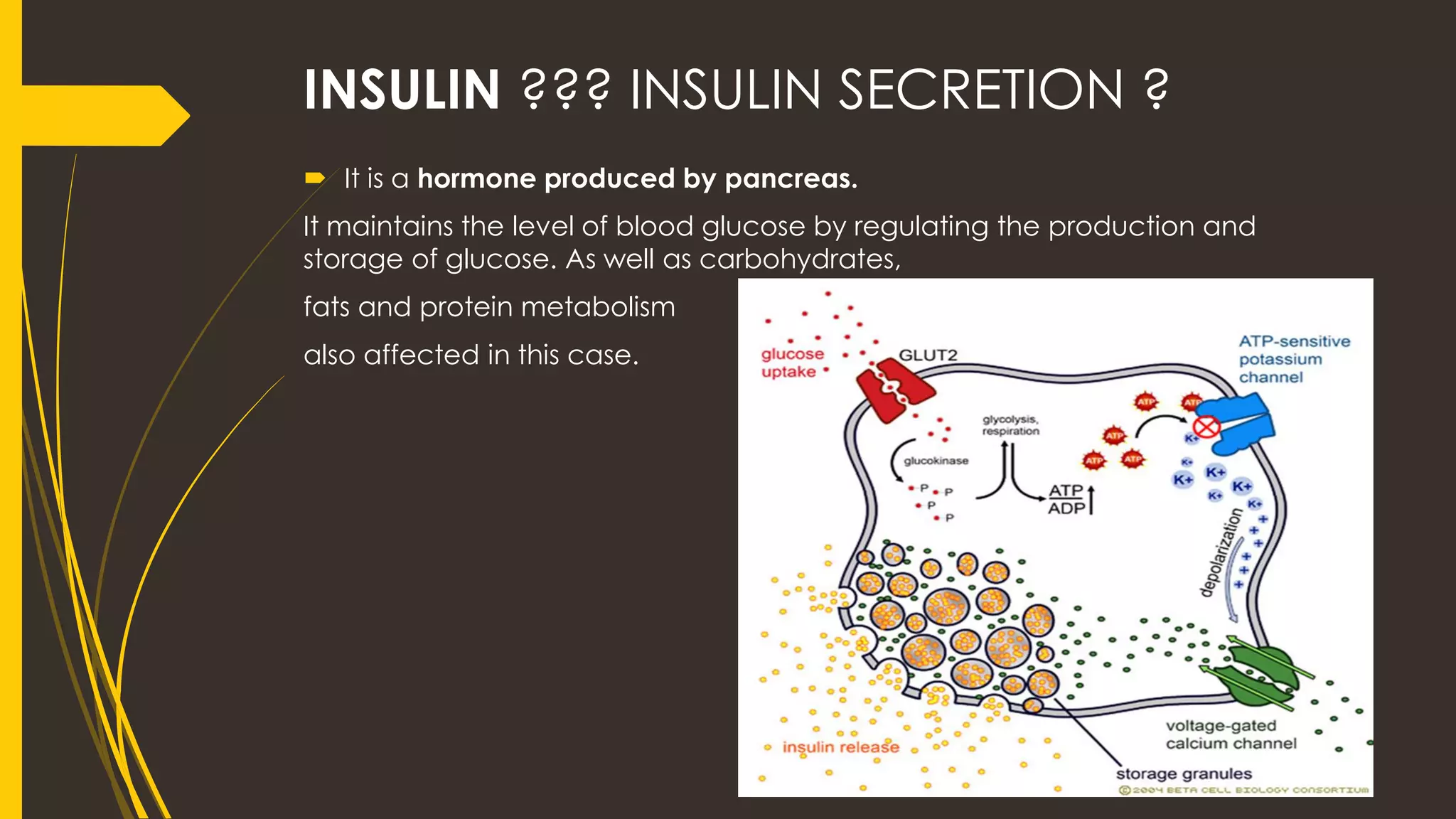
Diabetes mellitus is a disease characterized by high blood glucose levels due to the body's inability to produce or properly use insulin. There are two main types of diabetes - Type 1 is caused by an autoimmune destruction of insulin-producing beta cells, while Type 2 is associated with insulin resistance and impaired insulin secretion. Both types result in insufficient insulin and subsequent hyperglycemia. The document provides historical context on diabetes and outlines the roles of insulin, pancreatic hormones, and the metabolic processes involved in both healthy and diabetic states.










![TYPES OF INSULIN
TYPES OF INSULIN ONSET OF ACTION PEAK ACTION DURATION OF
ACTION
RAPID ACTION
INSULINS( lispro
[humalog] and
aspart [novolog]
5-20 minutes 30- 90 minutes 2-5 hours
REGULAR INSULIN 30-60 minutes 1 – 5 hours 6- 10 hours
INTERMEDIATE –
ACTING INSULIN ()
1-4 hours 6- 12 hours 12-24 hours
LONG –ACTING
INSULIN (protime
zinc ultralente
insulin )
4- 8 hours 16-18 hours up to to 30 hours](https://image.slidesharecdn.com/endocrinedisorder-diabetesmellitusdmbymr-200806112337/75/Endocrine-disorder-Diabetes-Mellitus-DM-12-2048.jpg)