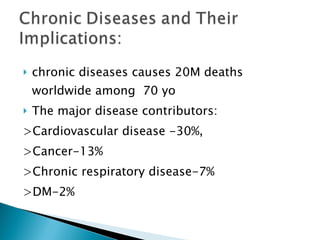
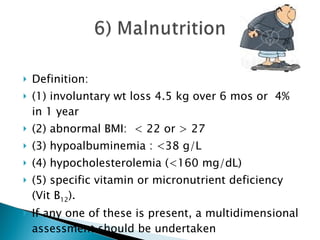
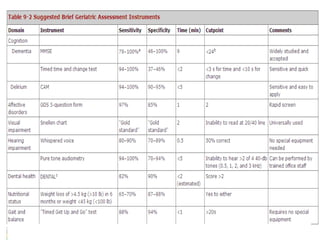
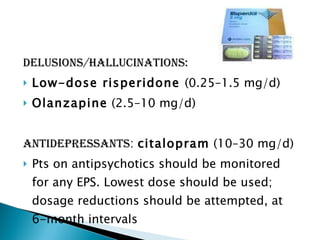
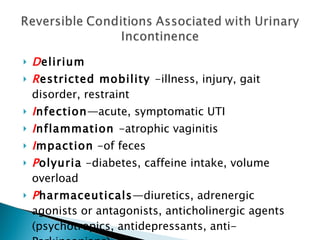
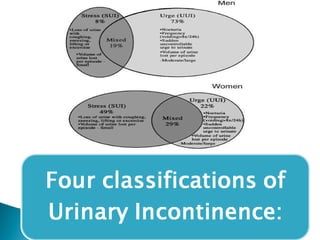
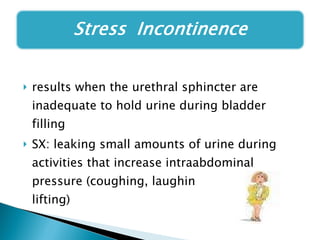
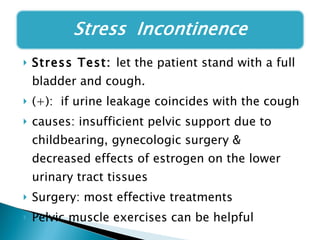
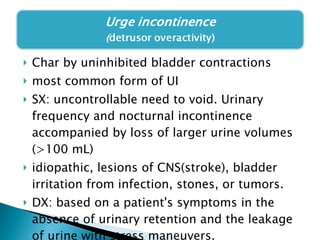
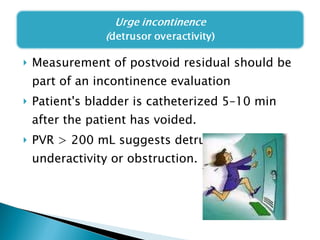
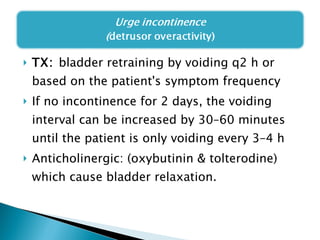
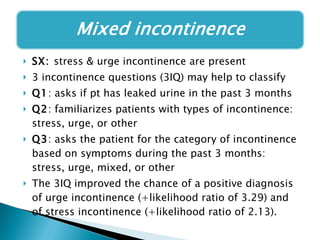
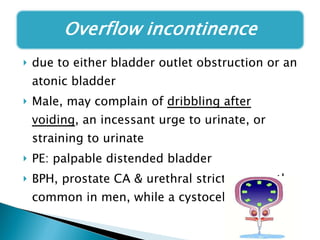
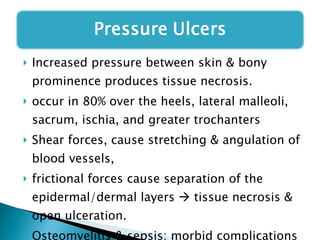
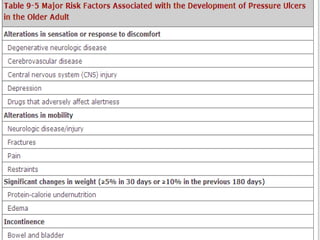
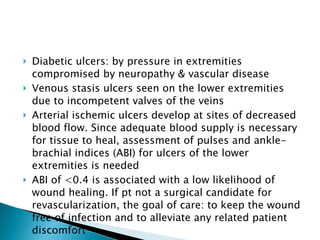
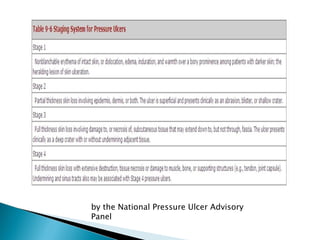
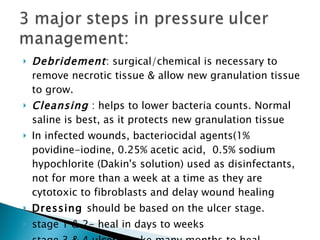
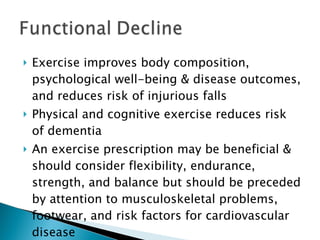
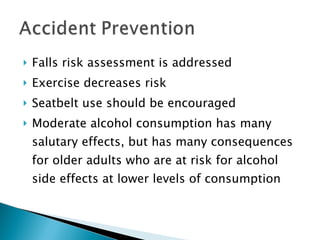
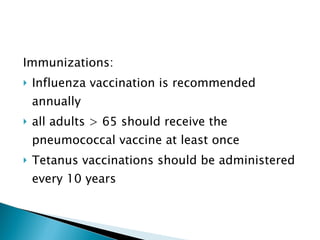
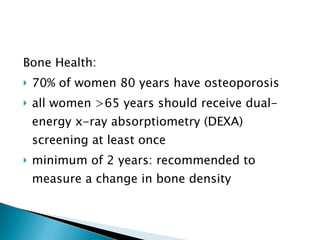
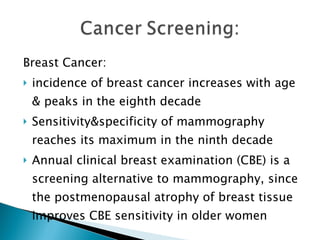
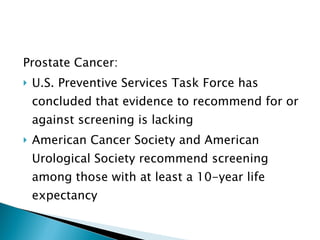
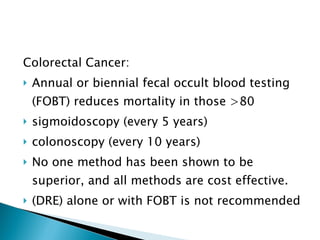
The document provides an overview of geriatrics, focusing on the medical care of older adults, including the assessment and management of physical, mental, and functional challenges they face. Key topics include the prevalence of chronic diseases, preventive measures, functional assessments, and the importance of addressing conditions such as dementia, delirium, and urinary incontinence. It emphasizes the need for comprehensive care to improve quality of life, including nutrition, exercise, and screening for various age-related diseases.