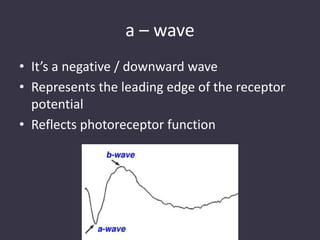
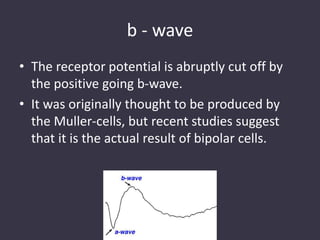
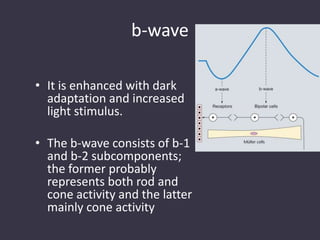
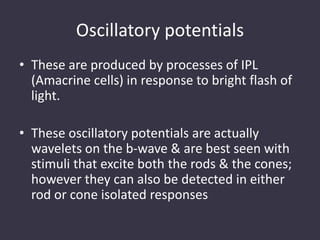
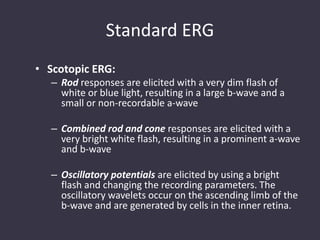
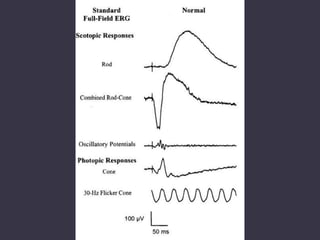
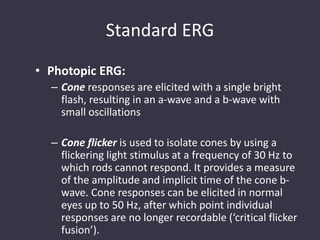
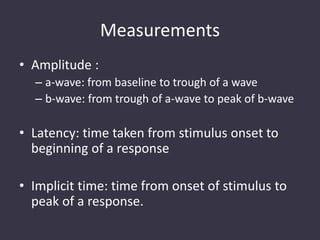
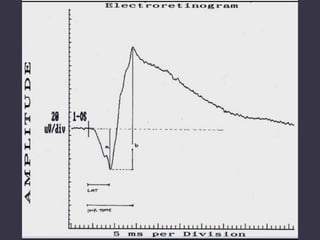
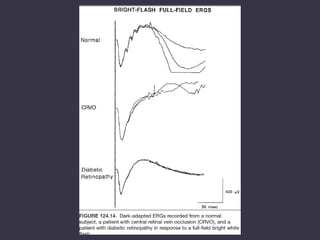
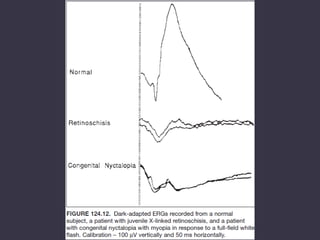
Electrophysiological tests like ERG, EOG, and VEP objectively assess retinal and visual pathway function, aiding in diagnosis of retinal diseases. ERG measures the retinal electrical response to flashes of light. It analyzes the a-wave from photoreceptors and b-wave from bipolar cells, with oscillatory potentials from amacrine cells. ERG can locate disease to the retina or visual pathway and quantify visual impairment over time. Diseases like diabetic retinopathy, glaucoma, and retinal degenerations impact ERG amplitudes and implicit times characteristically. ERG is a valuable test for evaluating retinal function.