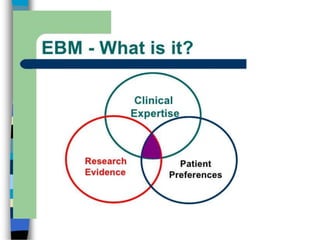
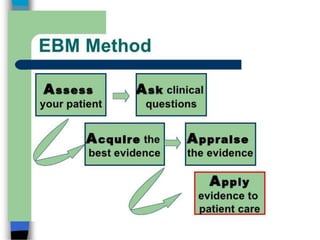
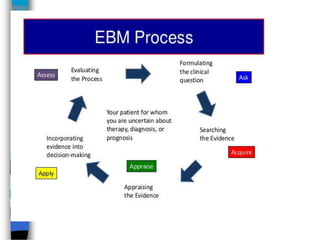
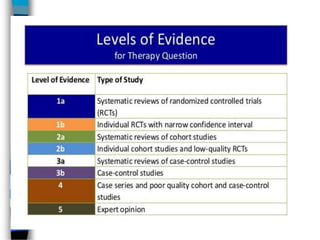
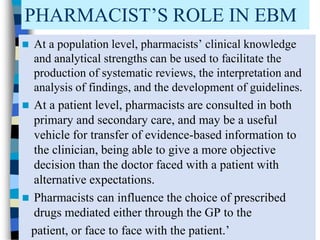
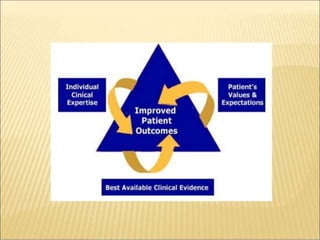
This document defines evidence-based medicine (EBM) and outlines its key aspects. EBM involves integrating the best available research evidence with clinical expertise and patient values. It teaches physicians to apply clinical and epidemiological research studies to patient care. EBM aims to make individual decision making more objective and evidence-based. Pharmacists can play an important role in EBM by facilitating systematic reviews, interpreting research findings, developing guidelines, and transferring evidence-based information to clinicians and patients.