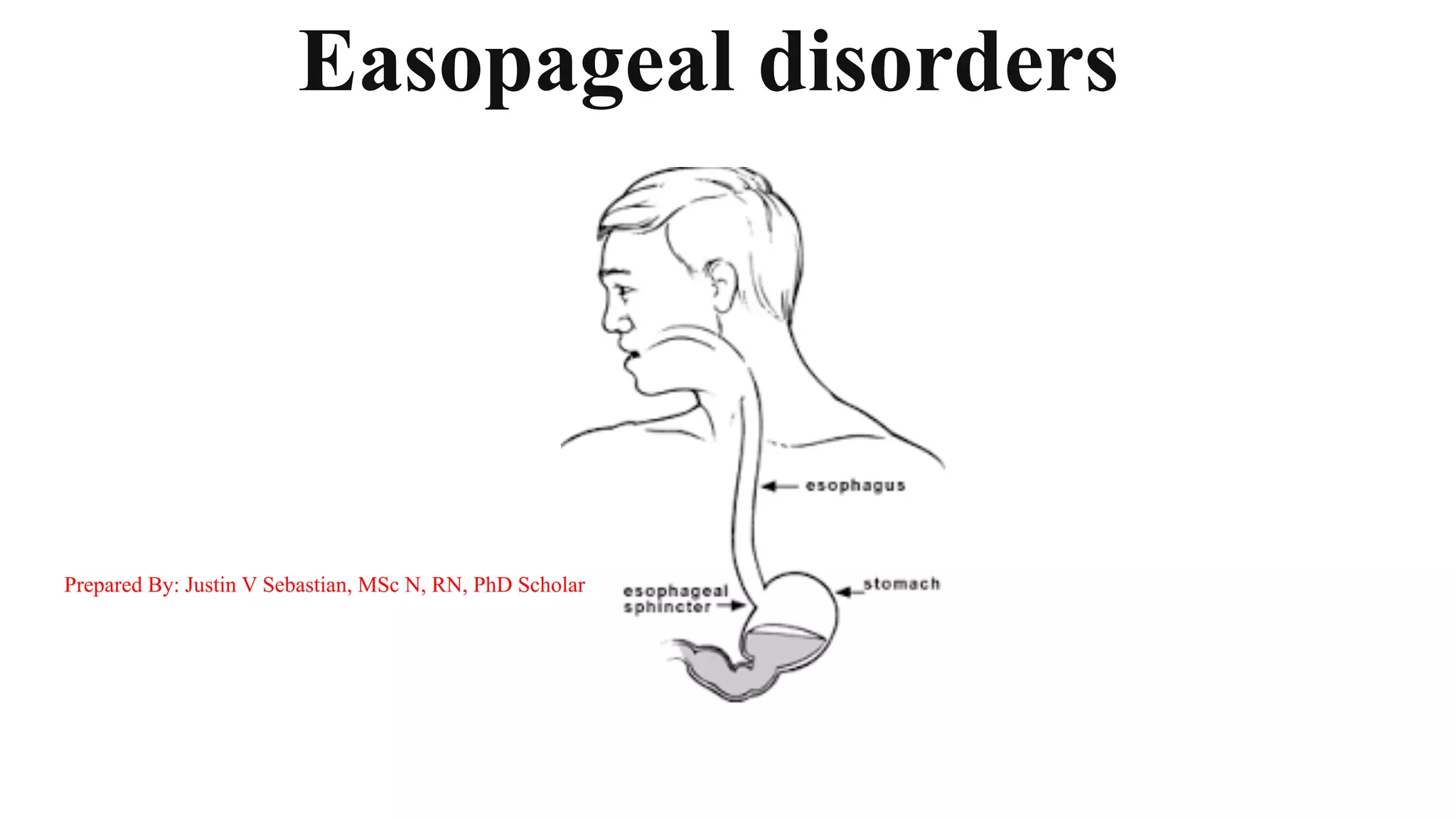
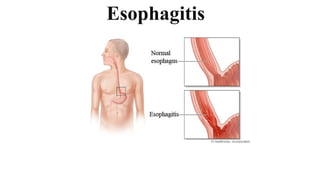
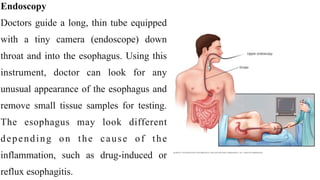
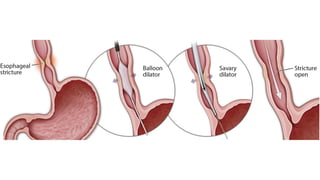
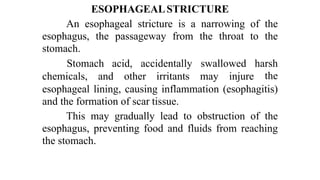
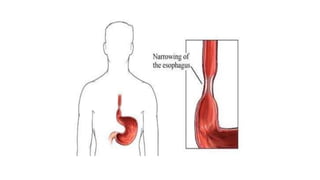
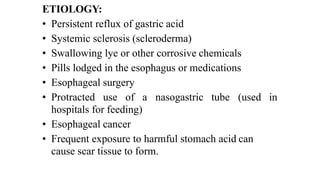
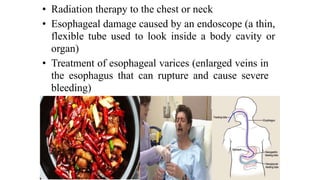
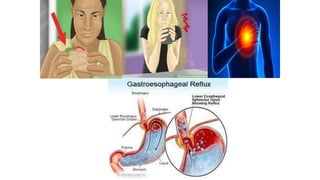
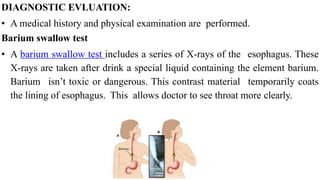
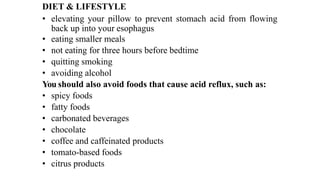
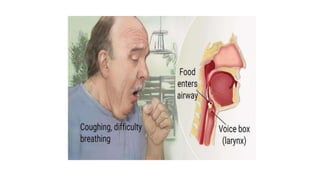
The document discusses esophageal disorders, specifically esophagitis and esophageal strictures. It defines esophagitis as inflammation of the esophagus that can be caused by acid reflux, eosinophilic esophagitis, lymphocytic esophagitis, certain drugs, and infections. Left untreated, esophagitis can lead to complications like esophageal strictures, which are narrowings of the esophagus caused by scarring. The document outlines signs, diagnostic tests, and treatment approaches for the different types of esophagitis.