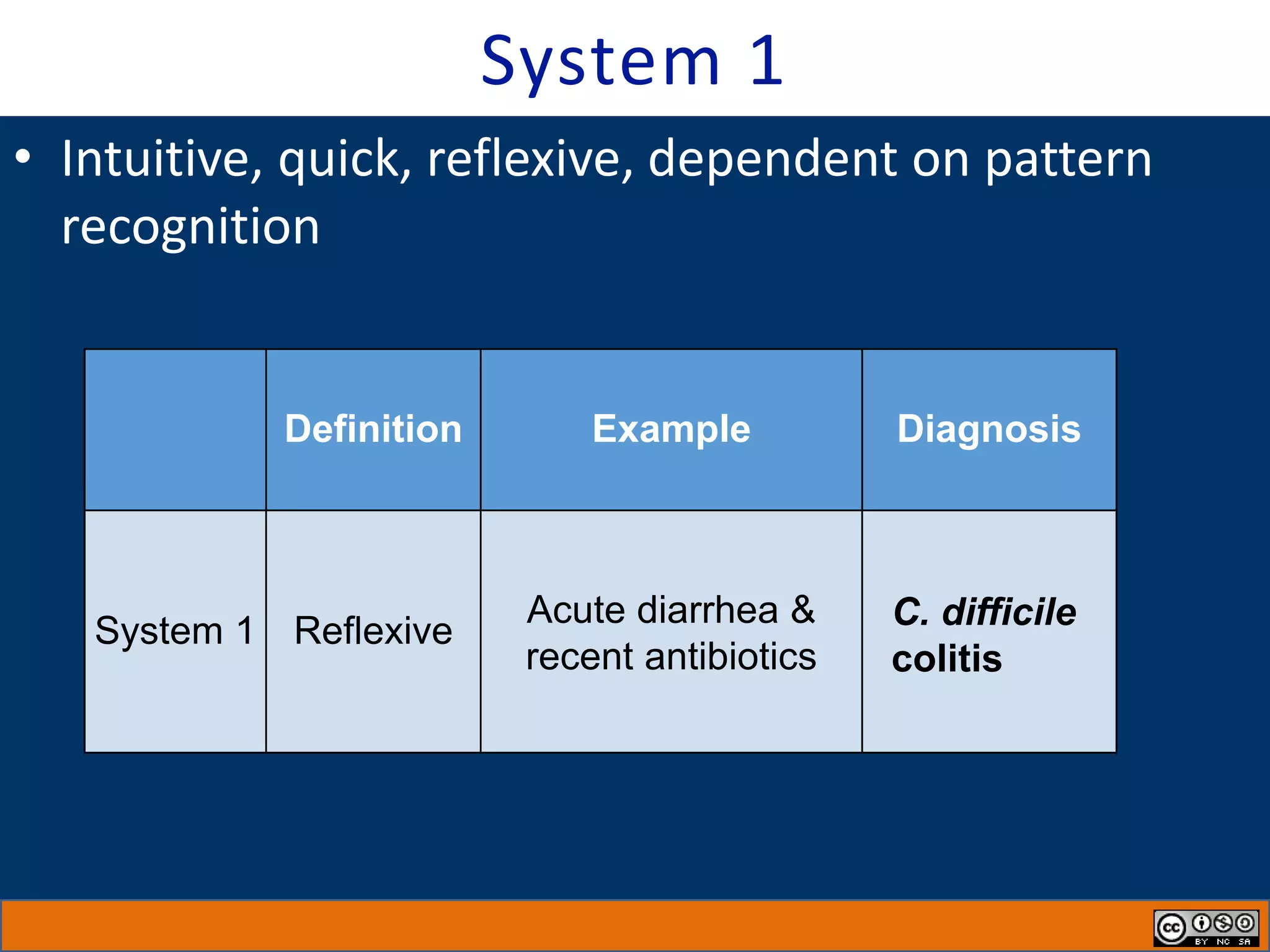
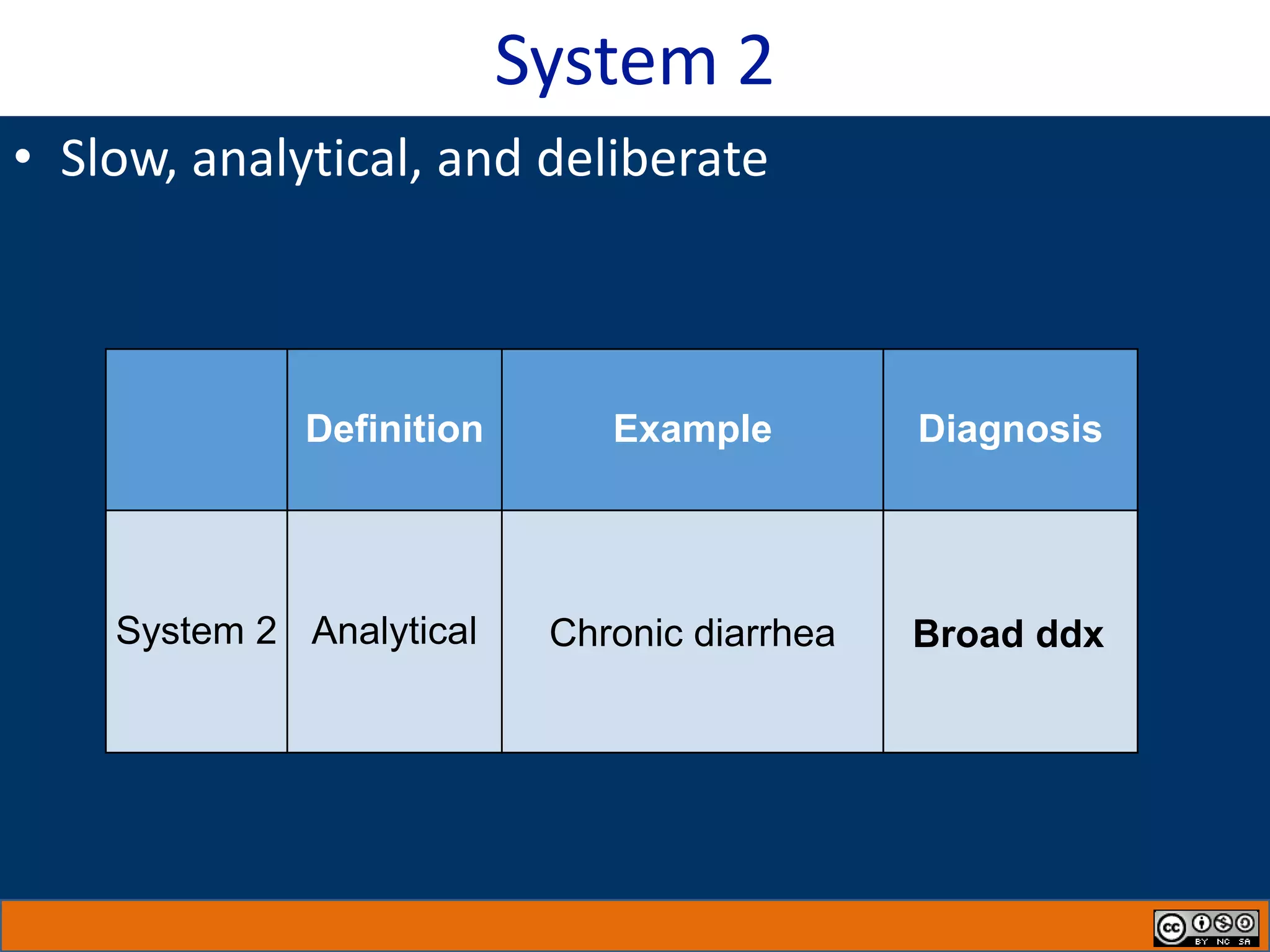
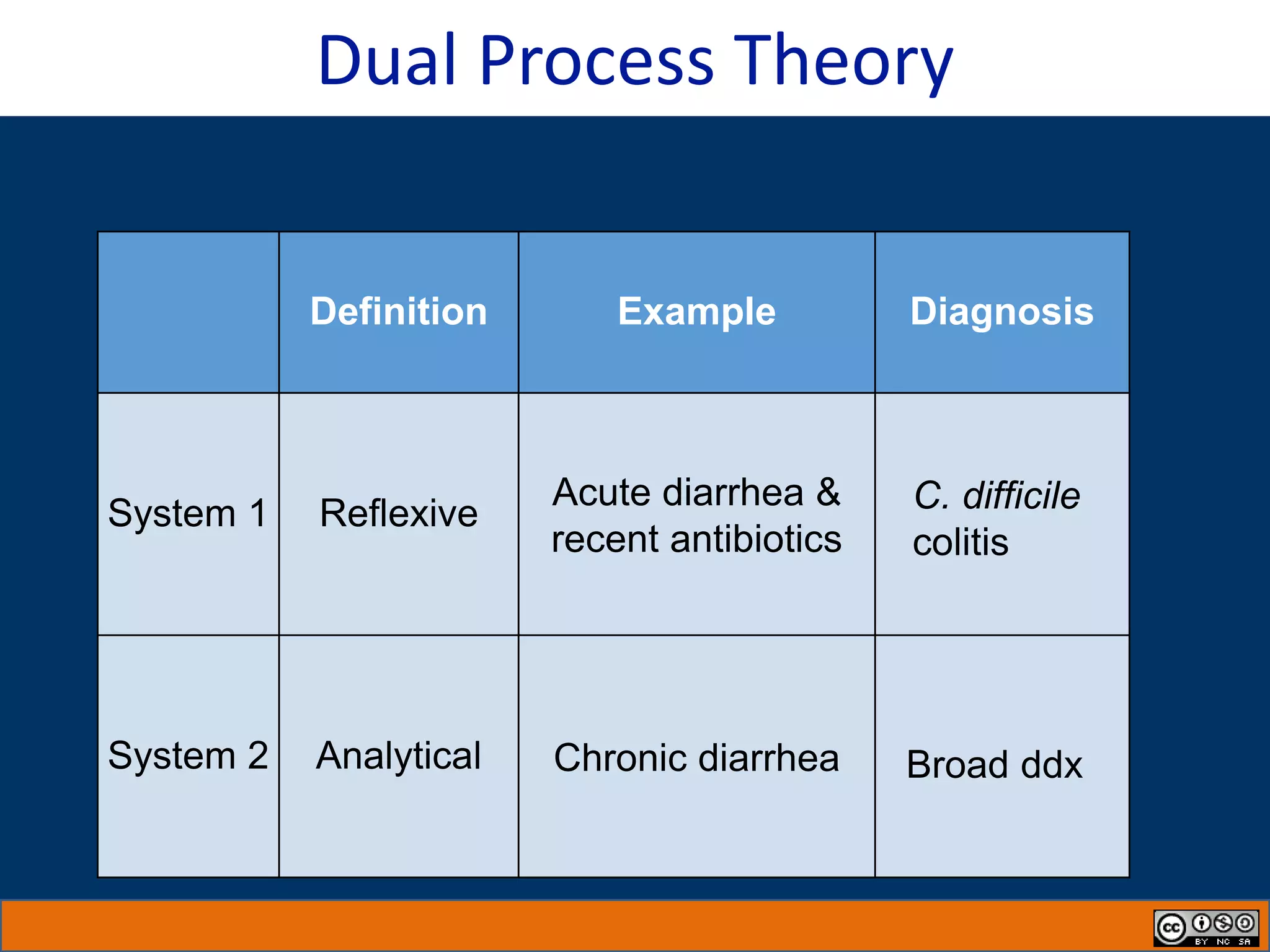
1) Dual process theory describes two modes of thinking: System 1 thinking is intuitive, quick, and based on pattern recognition. System 2 thinking is slow, analytical, and deliberate.
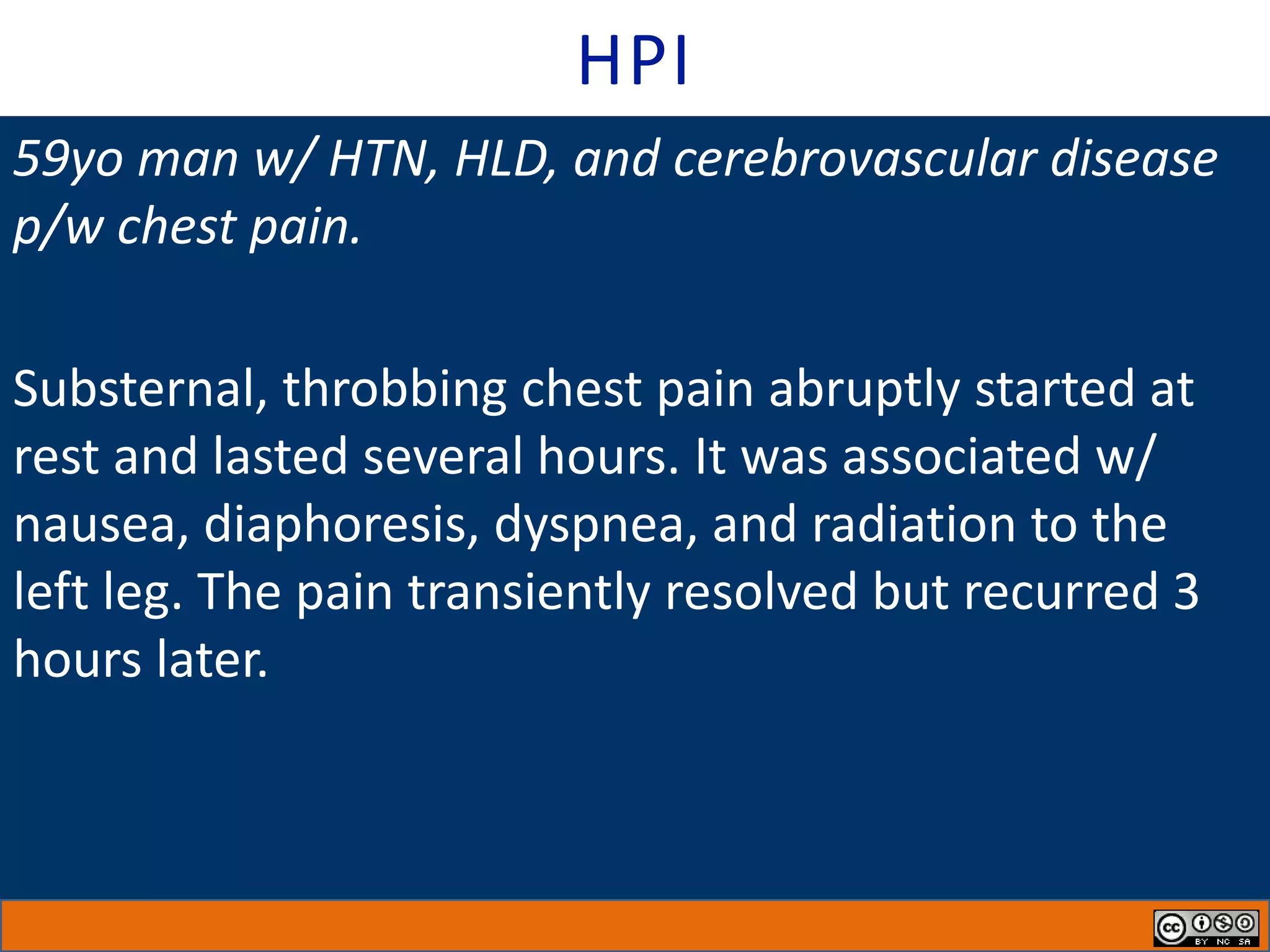
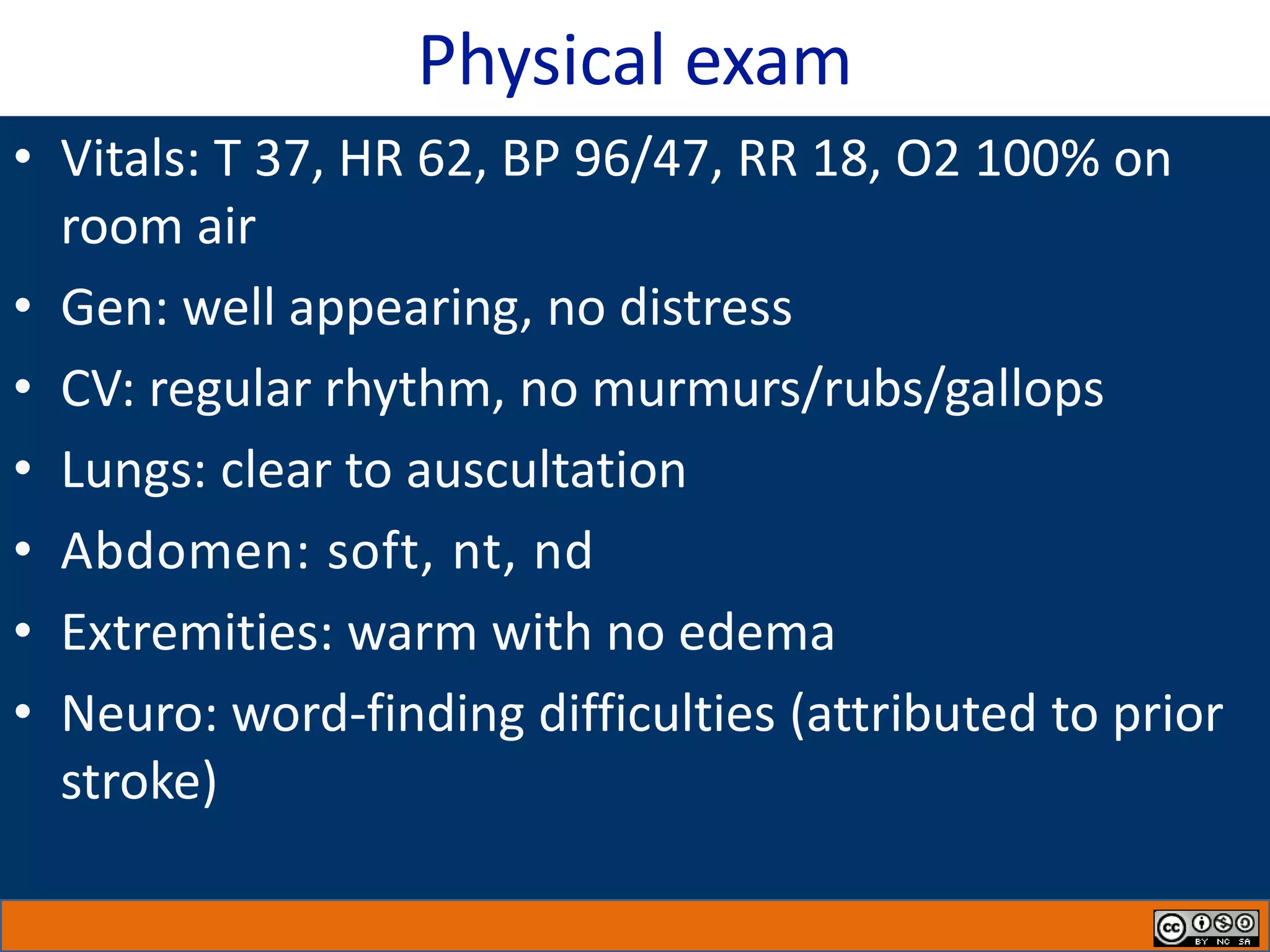
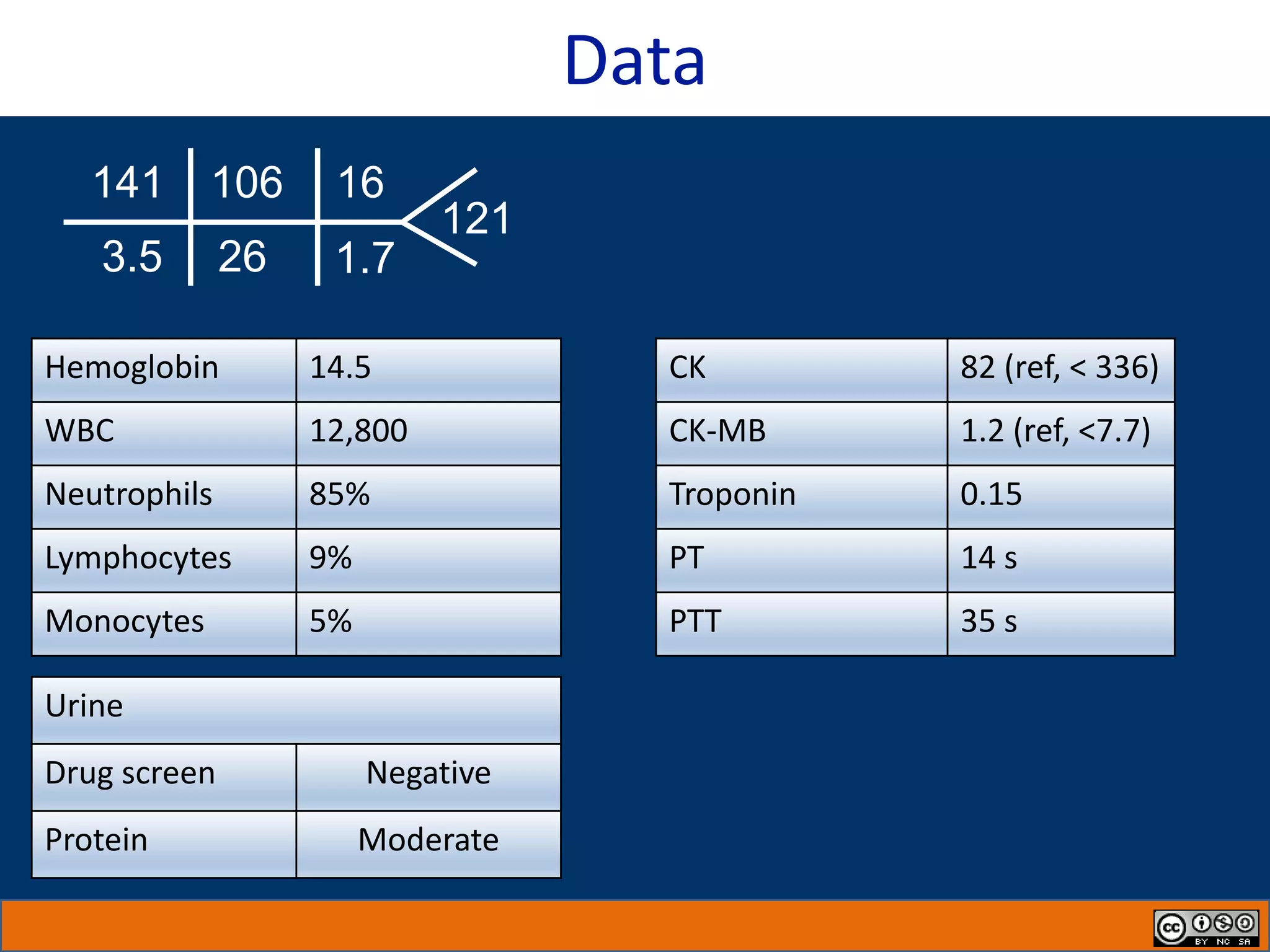
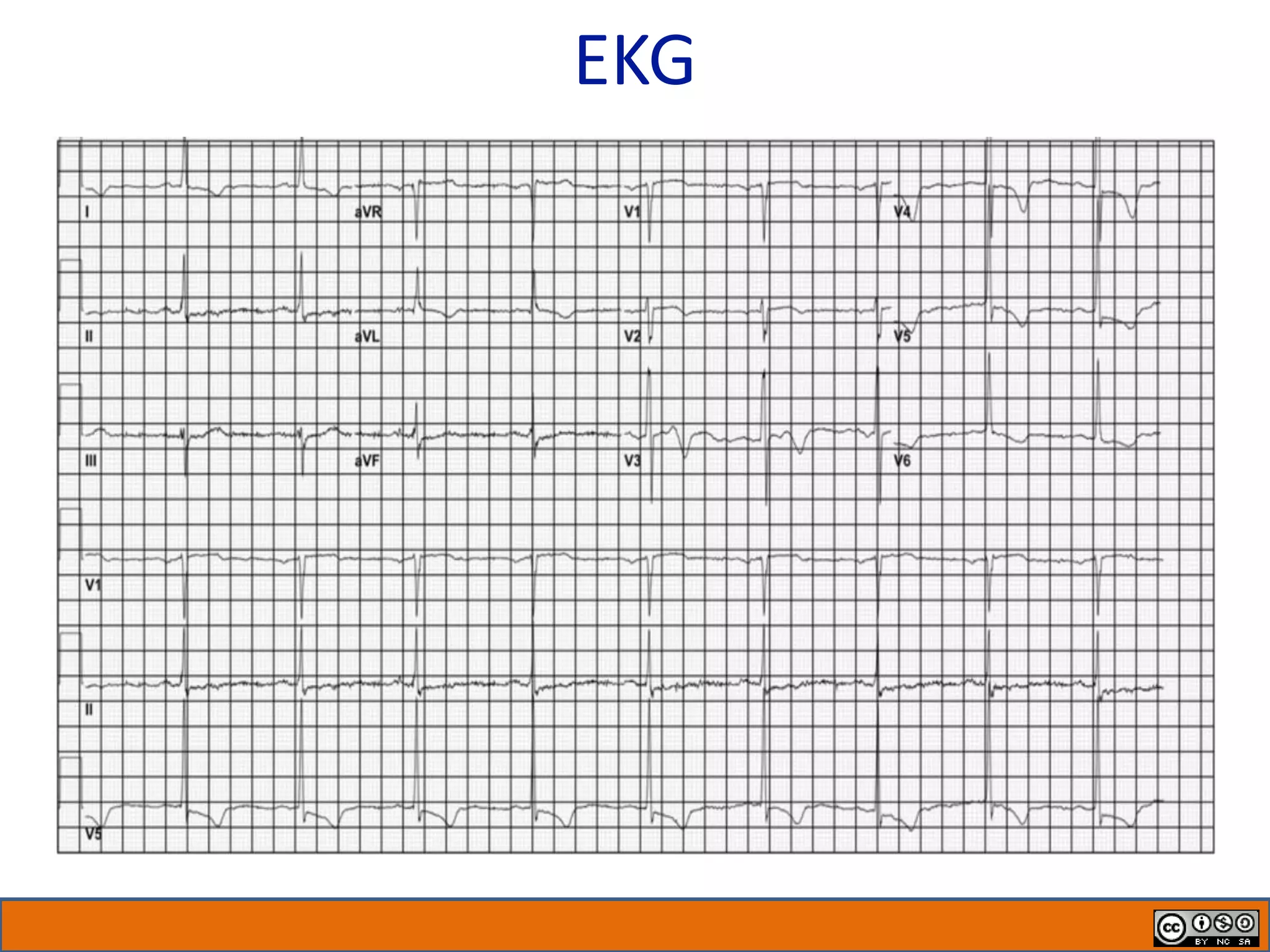
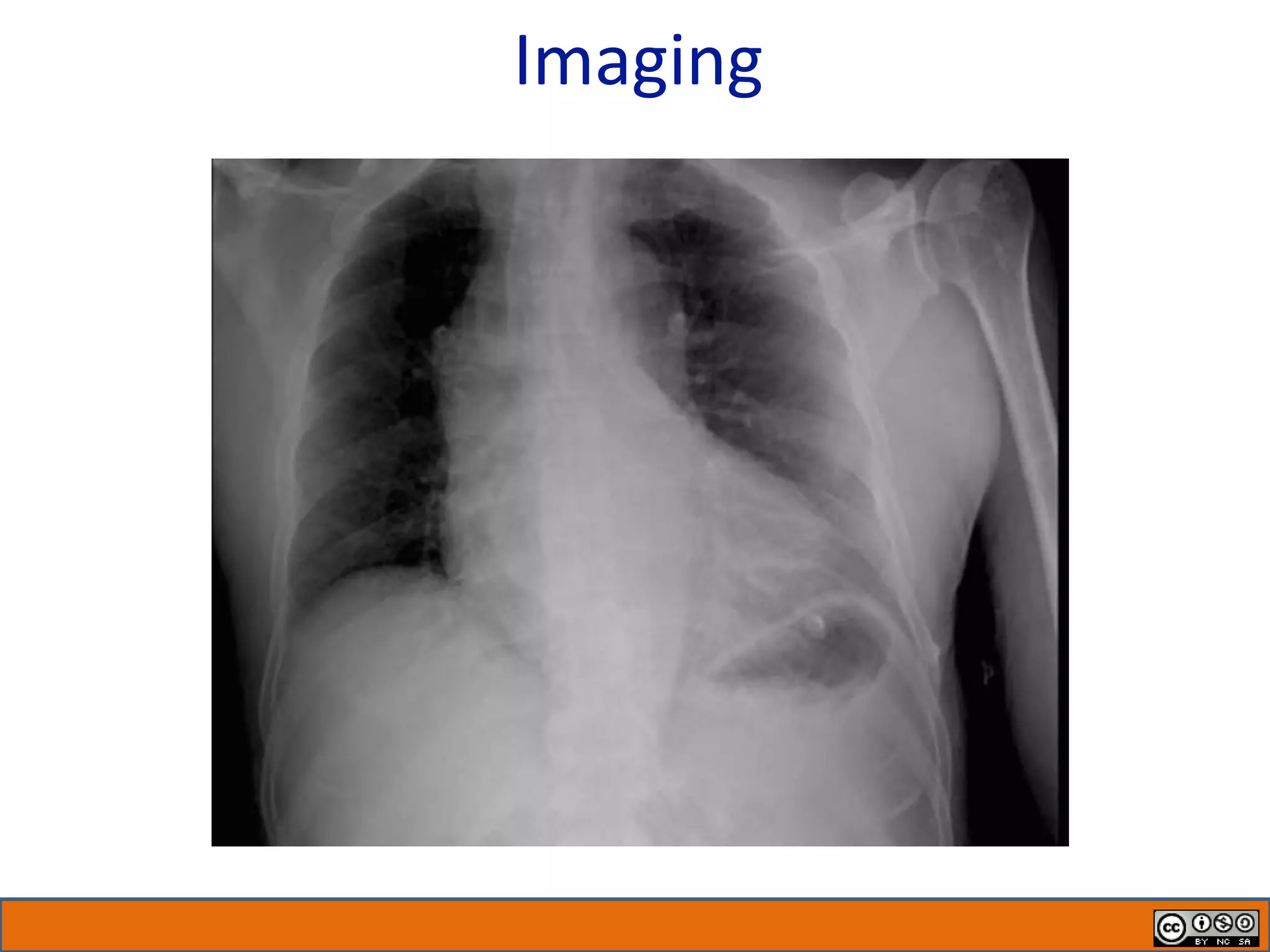
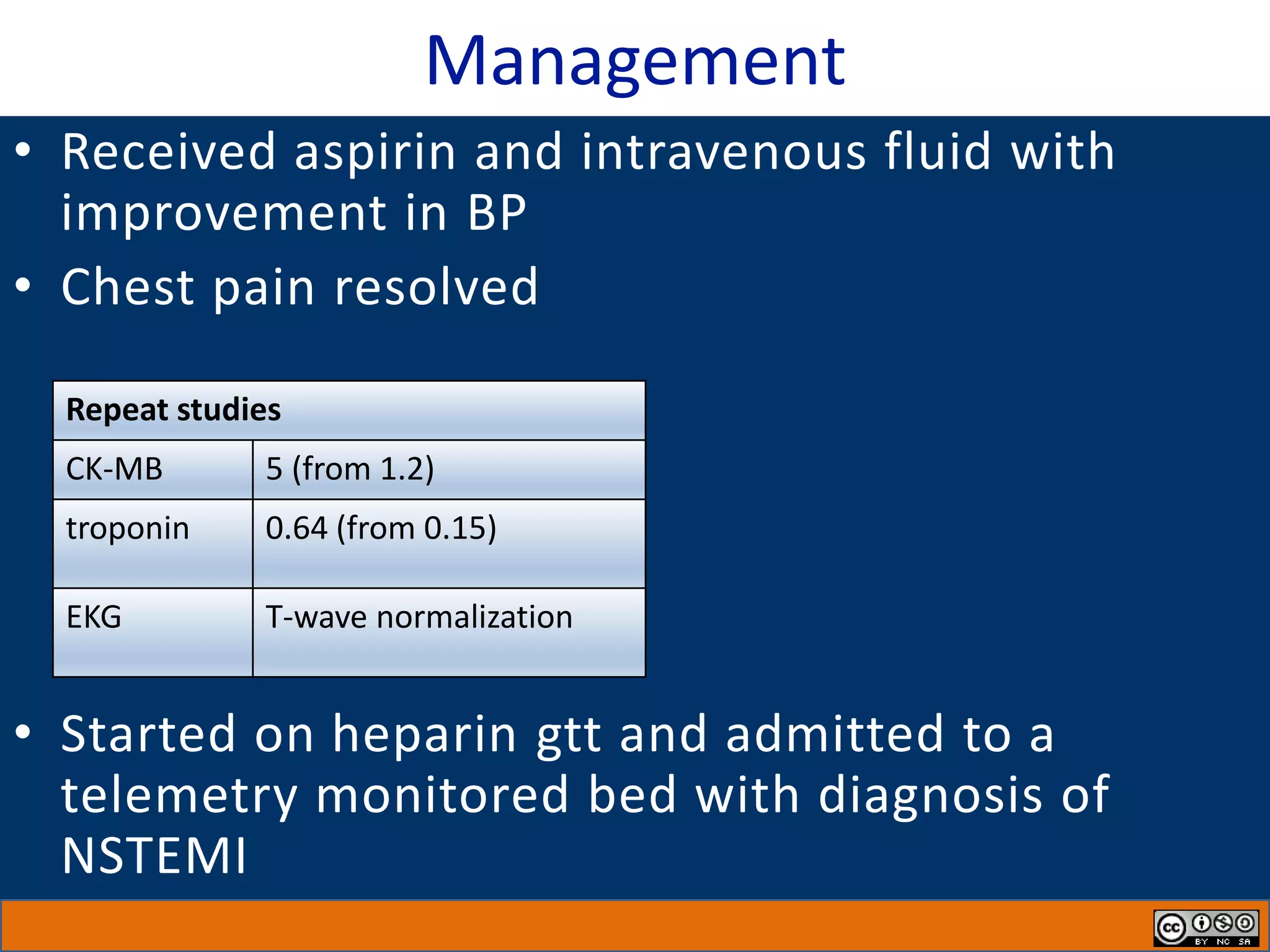
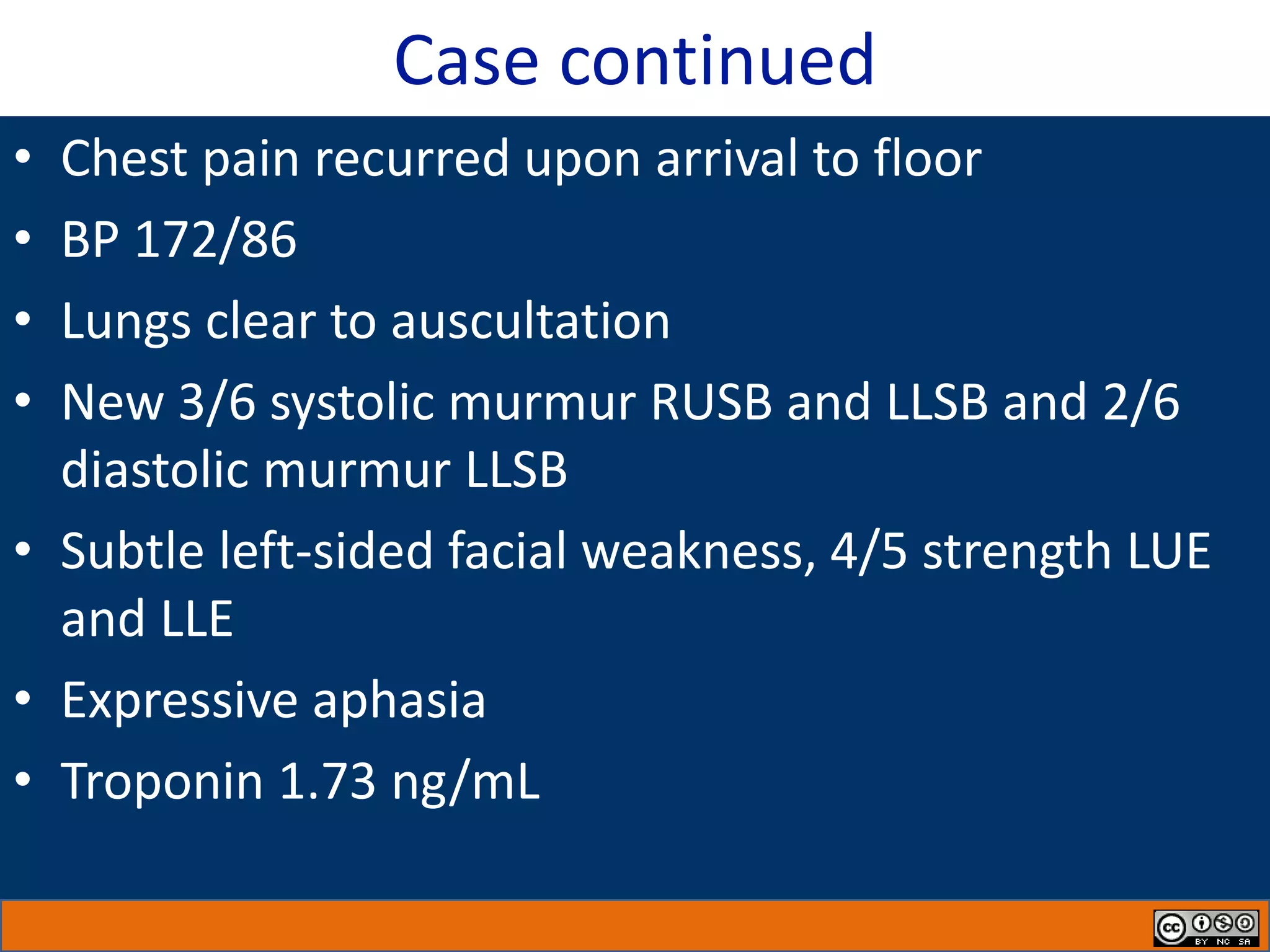
2) A 59-year-old man presented with chest pain and elevated cardiac troponin. Initial diagnosis was non-ST elevation myocardial infarction (NSTEMI) based on System 1 thinking.
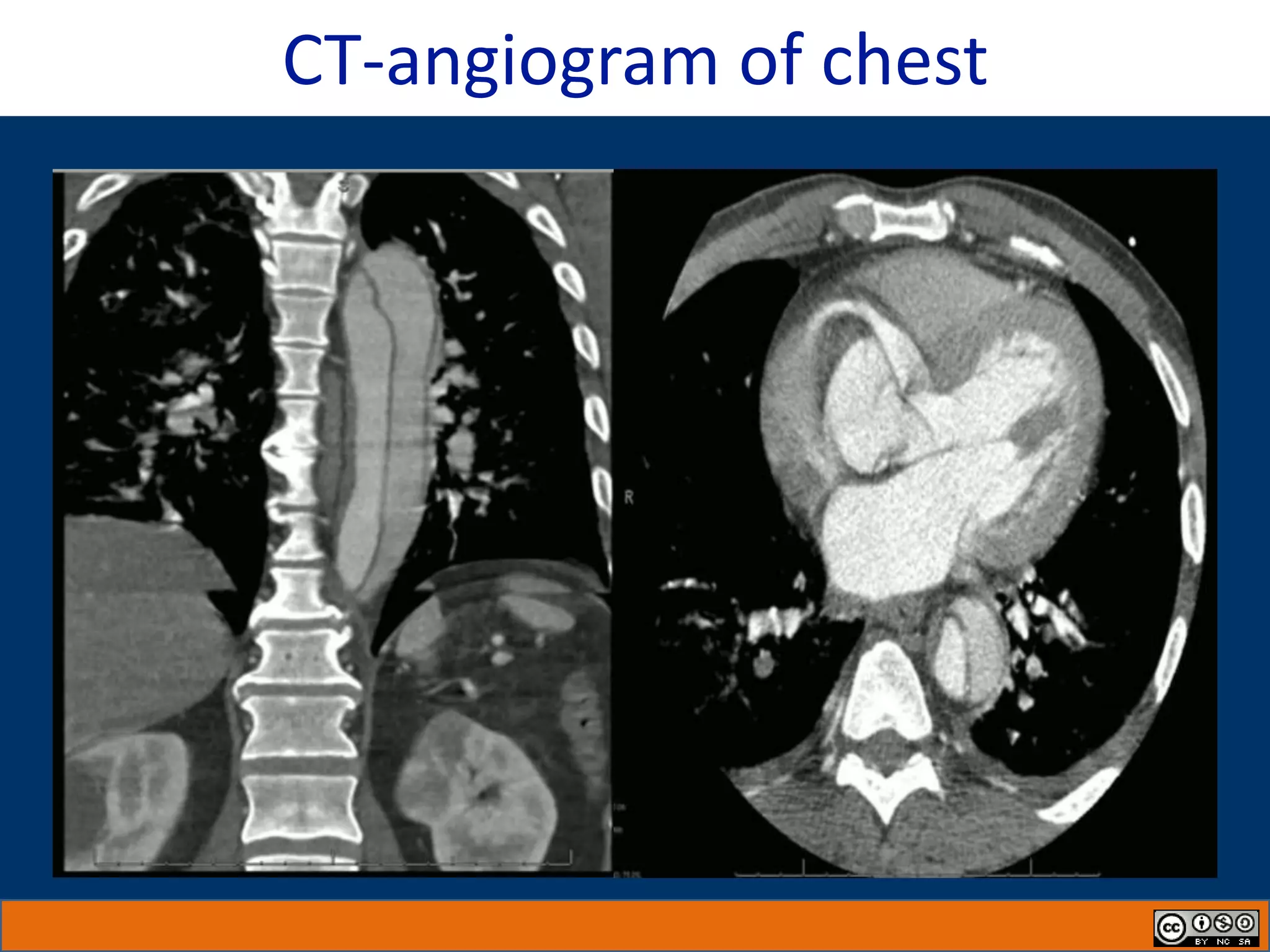
3) Further examination revealed new cardiac murmurs, neurological symptoms, and asymmetric blood pressure, inconsistent with NSTEMI. This triggered a transition to System 2 thinking and a new diagnosis of aortic dissection was made.