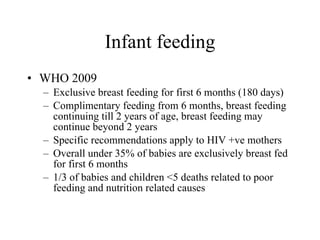
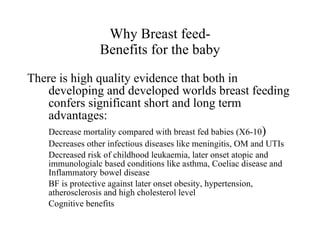
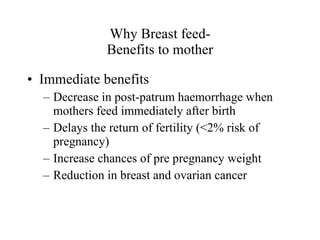
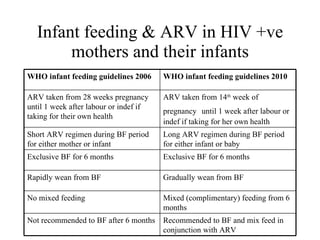
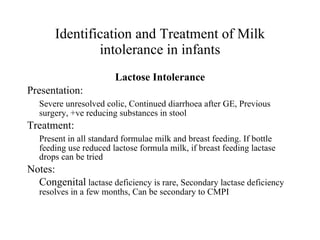
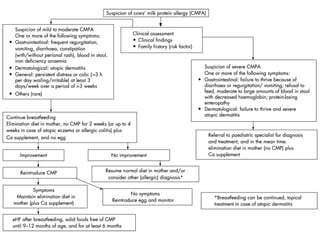
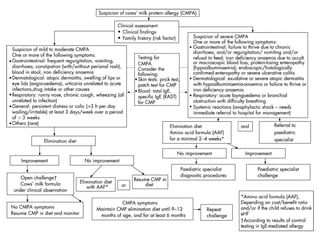
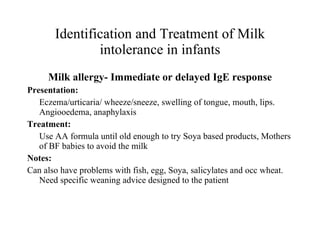
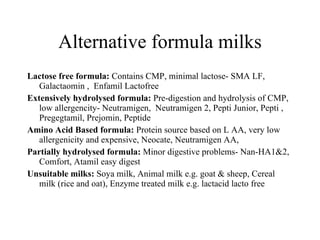
This document discusses infant feeding and intolerances. It provides recommendations from the WHO on exclusive breastfeeding for 6 months and continuing breastfeeding until 2 years of age. It also discusses the benefits of breastfeeding for both babies and mothers. The document then covers types of milk intolerances such as protein and lactose intolerance. It describes the identification and treatment of various milk intolerances in infants.