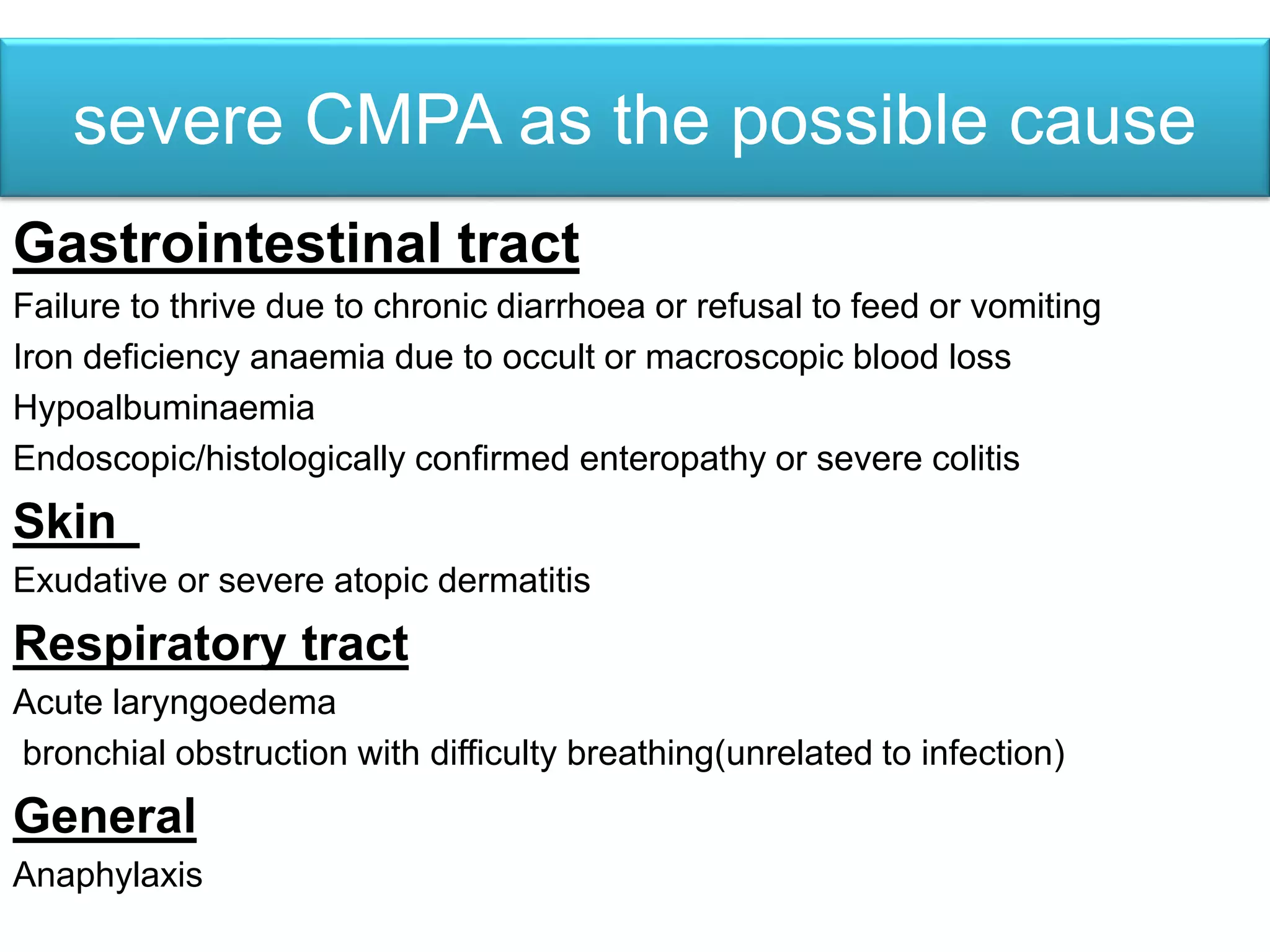
Cow's milk protein allergy (CMPA) is the leading cause of food allergy in infants and young children, affecting approximately 5-15% of infants. Breastfeeding reduces the risk of CMPA to around 0.5% compared to formula-fed infants who have a higher risk. CMPA results from an immune reaction to proteins in cow's milk and can cause symptoms in the gastrointestinal, skin, and respiratory systems. Diagnosis involves an elimination diet and oral food challenge. Extensively hydrolyzed formulas are recommended for mild-moderate CMPA, while amino acid-based formulas are used for severe cases.