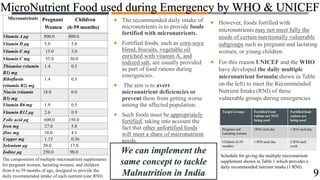
The document discusses ways to tackle malnutrition in India through a proposed micro-nutrient nutrition program. It notes that over 30% of India's population suffers from calorie-protein and micronutrient deficiencies. The program would provide multiple vitamin and mineral supplements to pregnant and lactating women and children aged 6-59 months. It outlines the composition of supplements designed to provide daily recommended nutrient intake. The program aims to address malnutrition across generations in a coordinated manner through supplements, fortified foods, and public awareness campaigns.