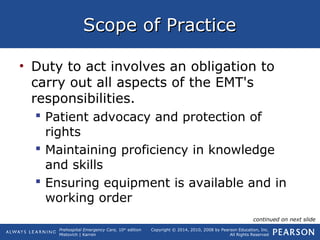
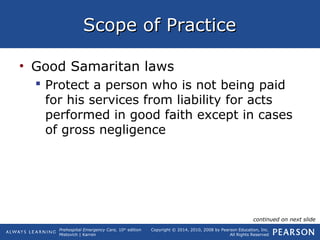
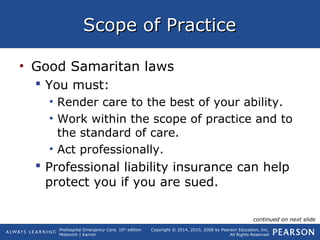
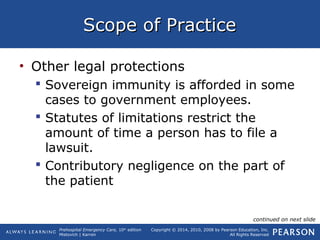
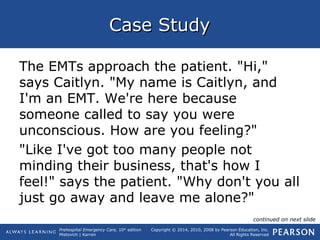
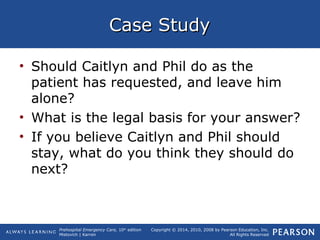
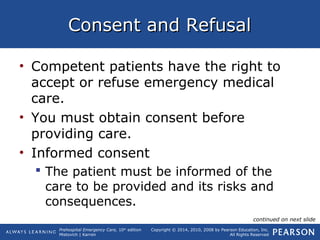
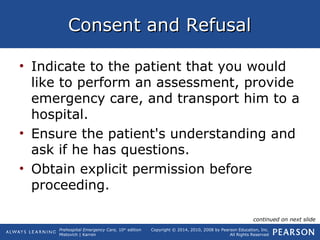
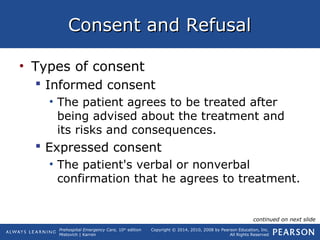
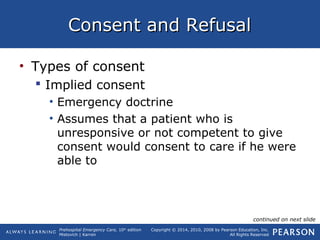
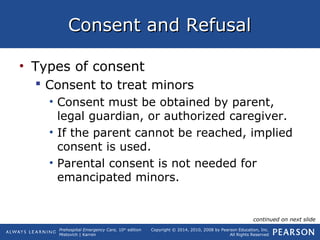
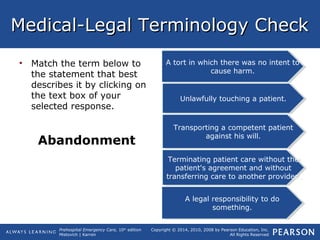
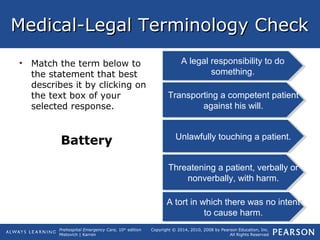
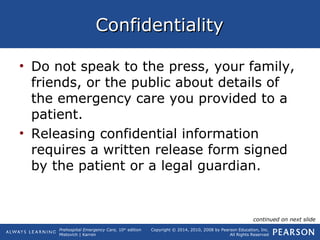
This document provides an overview of the key concepts around the scope of practice and legal/ethical issues that EMTs may face. It discusses topics like obtaining consent, a patient's right to refuse care, implied consent in emergencies, and advance directives. The document uses examples and case studies to illustrate how these concepts apply in the field. It emphasizes that EMTs have both legal and ethical obligations to provide care while respecting patient autonomy and acting in their best interests.