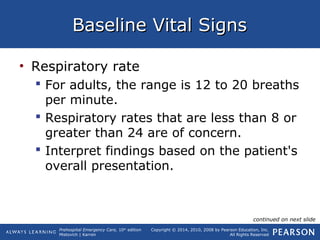
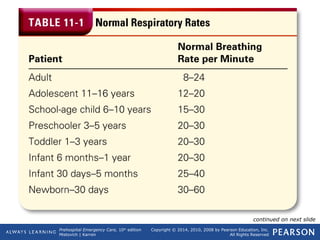
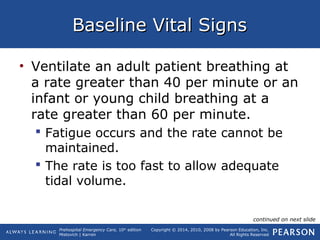
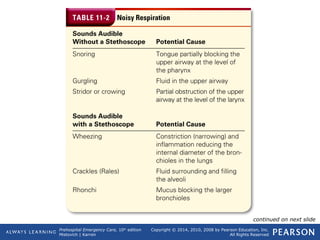
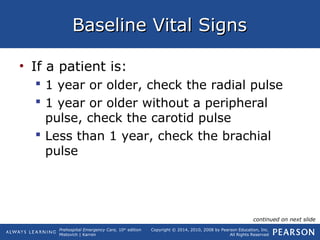
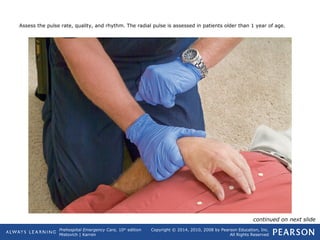
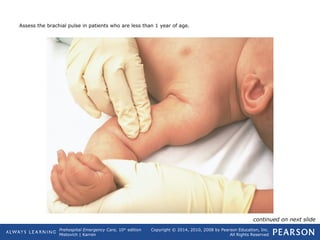
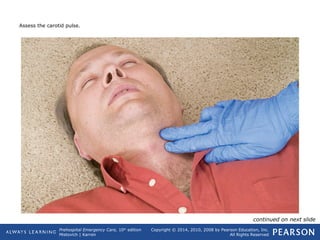
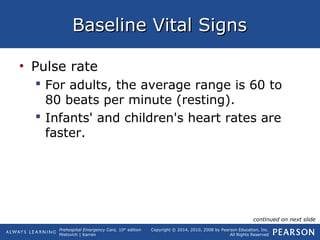
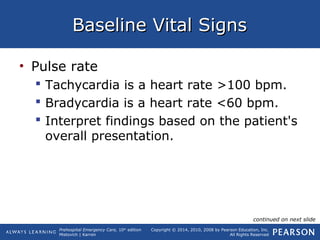
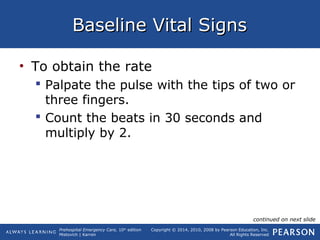
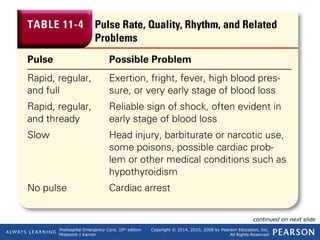
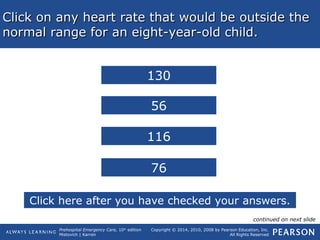
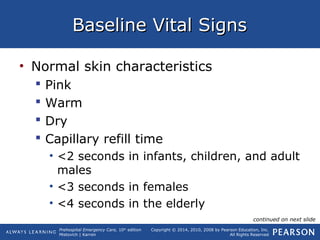
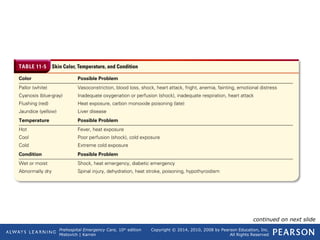
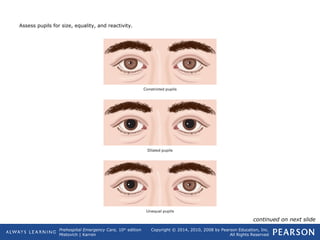
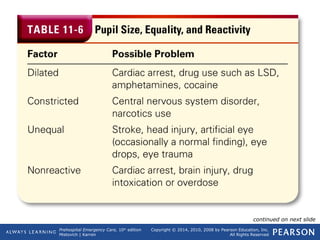
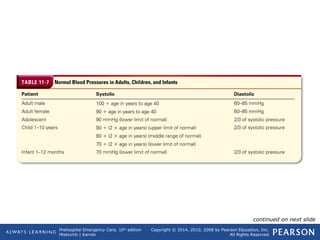
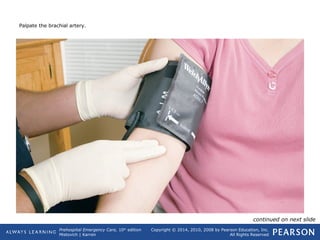
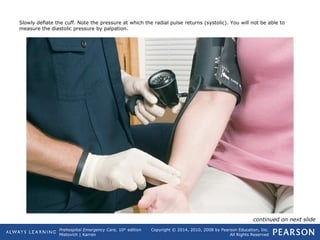
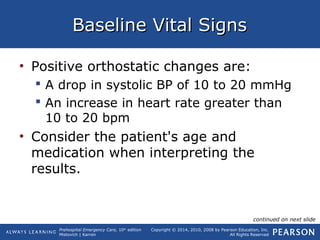
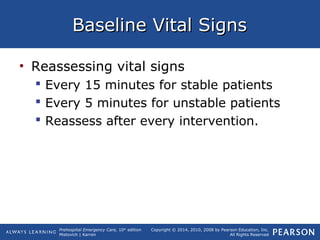
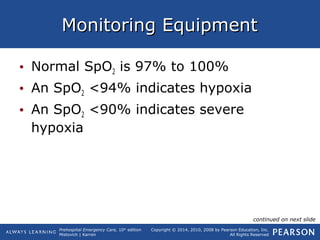
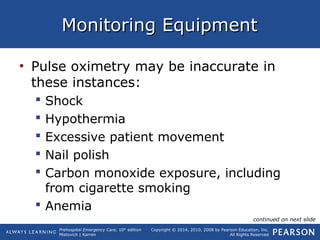
This document provides an overview of assessing baseline vital signs in prehospital emergency care settings. It discusses gathering information about a patient's condition upon arrival and measuring their initial respiration rate, pulse, skin appearance, pupil assessment, and blood pressure. Normal ranges for each vital sign are provided for adults, children and infants. The document emphasizes the importance of comparing later vital sign measurements to the initial baseline to detect any changes in a patient's condition over time.