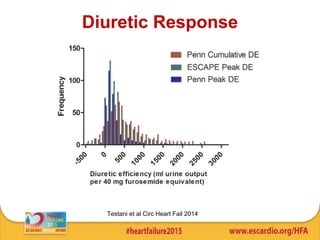
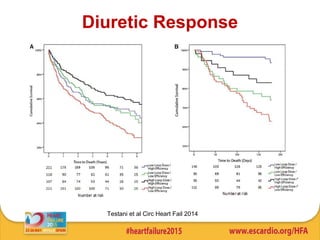
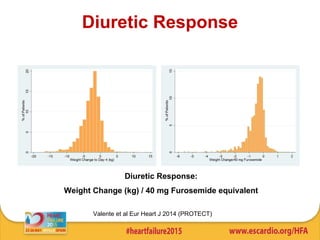
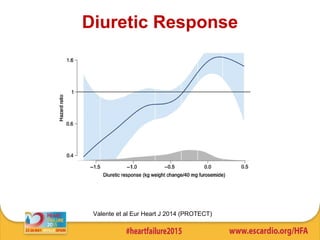
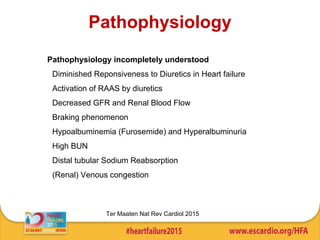
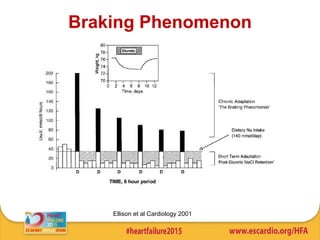
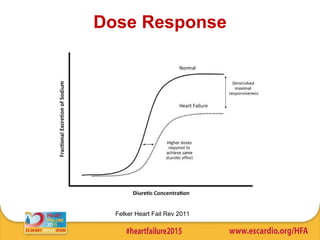
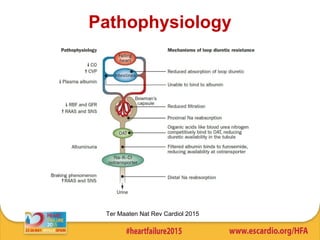
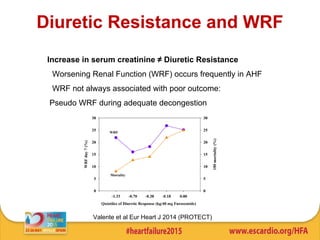
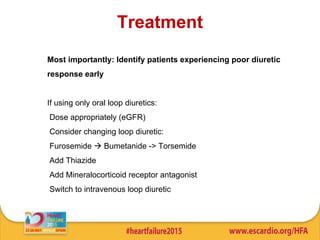
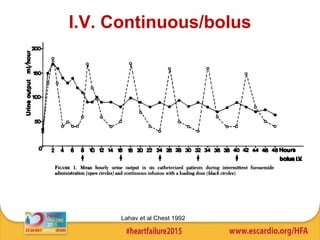
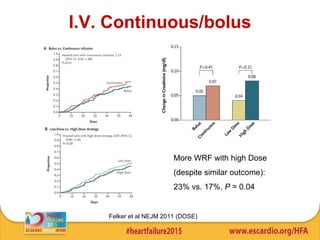
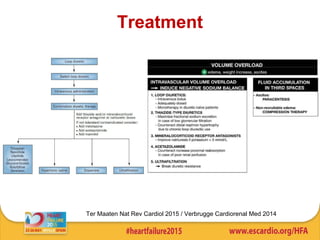
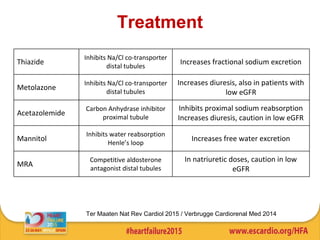
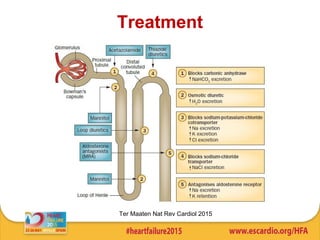
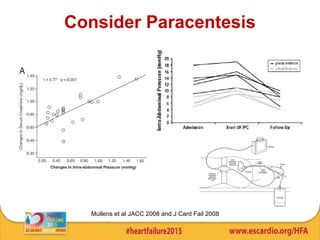
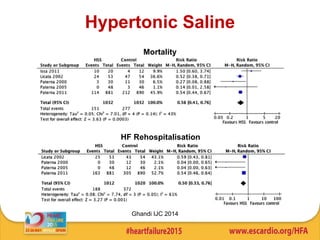
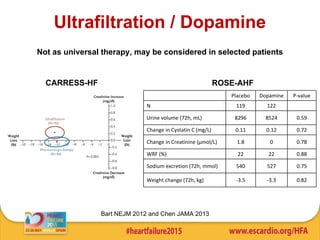
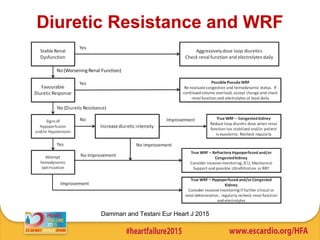
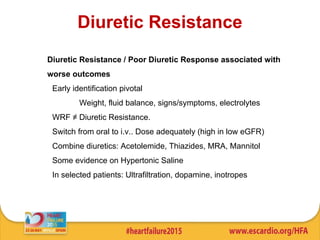
This document discusses challenging cases of acute heart failure involving diuretic resistance. It begins by defining diuretic resistance as a poor response to diuretic therapy, characterized by persistent signs and symptoms despite treatment. The pathophysiology of diuretic resistance is incompletely understood but may involve factors like RAAS activation, decreased renal function and blood flow, and distal tubular sodium reabsorption. The document reviews potential treatments for diuretic resistance including increasing and switching diuretic medications, adding mineralocorticoid receptor antagonists or thiazides, intravenous diuretic administration, and in select cases ultrafiltration. Early identification of diuretic resistance is important and associated with worse patient outcomes.