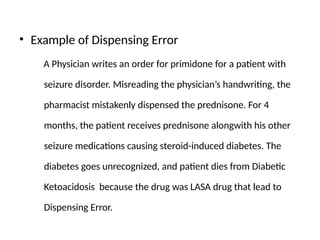
The document discusses the multidimensional nature of medication errors, their types (prescribing, dispensing, and administration), and contributing factors such as human, system, and medication-related issues. Recommendations are provided for reducing these errors, including electronic prescribing, thorough communication, and proper training for healthcare professionals. It highlights the significant role of regulatory authorities, prescribers, pharmacists, and nursing staff in preventing errors and ensuring patient safety.