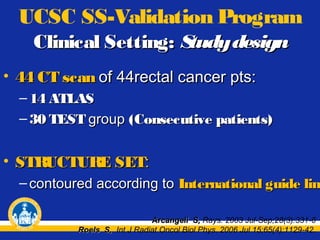
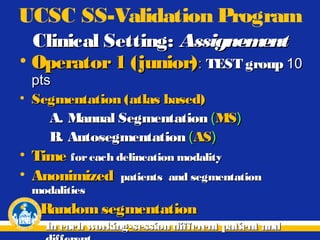
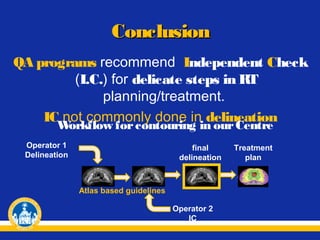
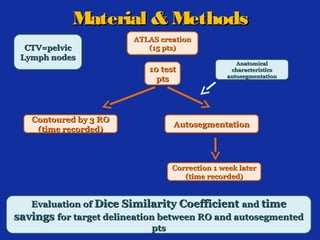
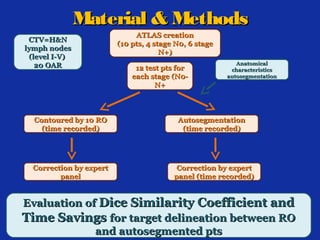
• Creation of 1 ATLAS
based on 15 pts
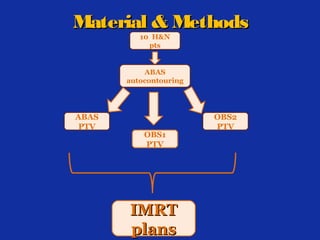
• 10 pts evaluated
- Autocontours breast CTV
- Autocontours breast PTV
- Autocontours OARs
- Autocontours pelvic
lymph nodes CTV
- Autocontours OARs
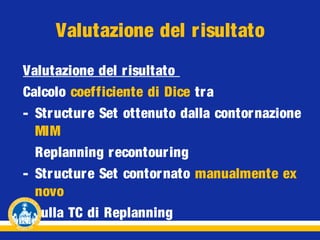
Evaluation:
Evaluation:
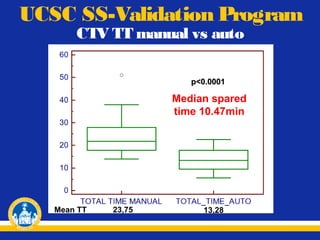
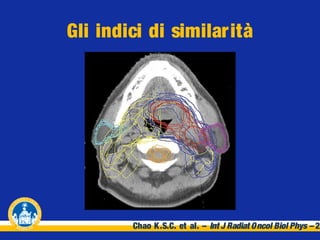
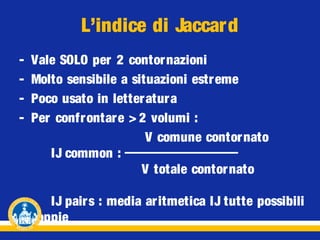
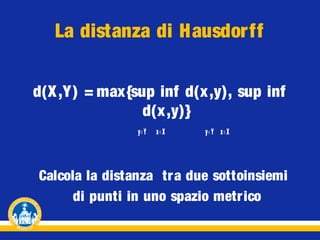
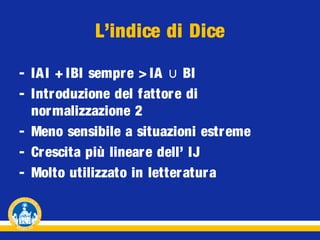
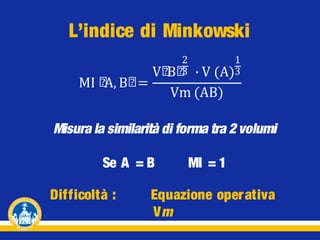
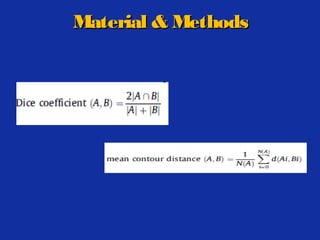
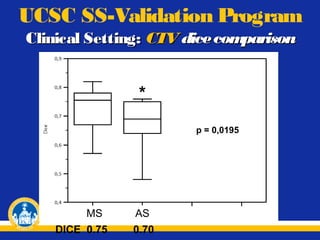
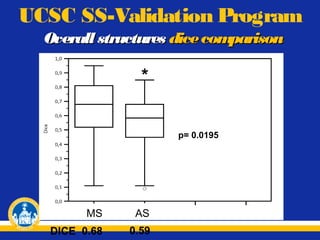
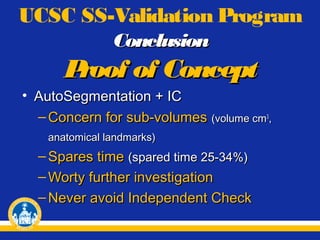
- Dice Similarity Coefficient
- Time savings
- Dice Similarity Coefficient
- Time savings
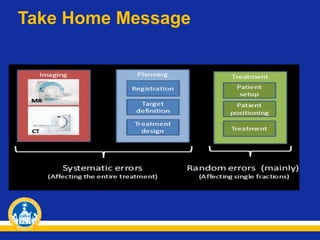
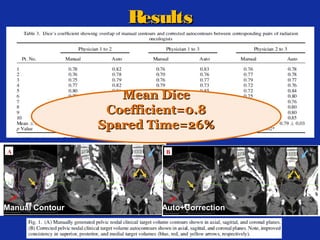
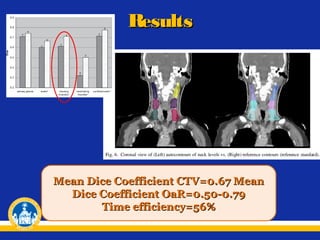
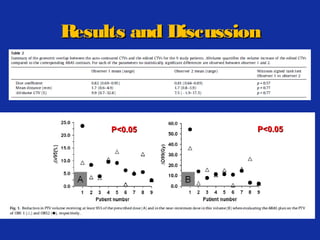
�Results
Breast Cancer
Anorectal Cancer
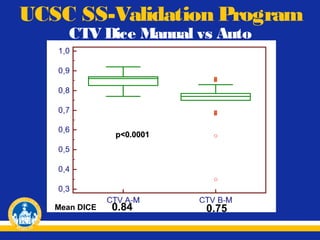
Mean Dice Coefficient:
Mean Dice Coefficient:
CTV = 0.85
PTV = 0.80
OARs = 0.75
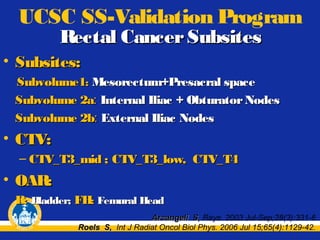
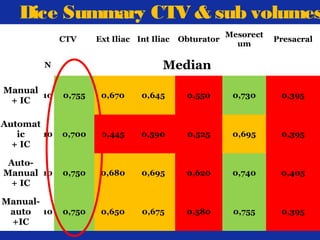
CTV








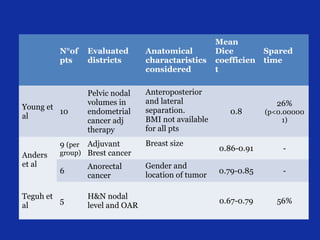

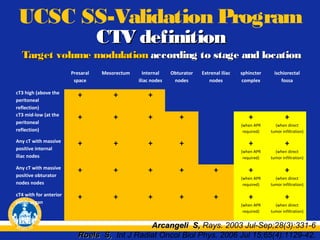
![N°of
pts
Evaluated
districts
Anatomical
charactaristics
considered
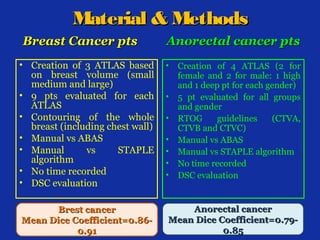
10
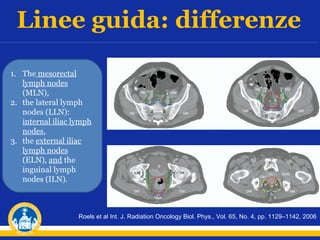
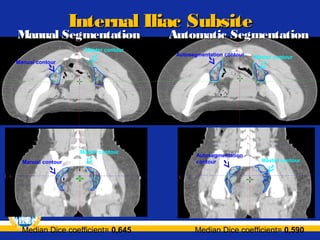
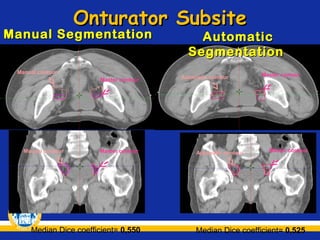
Pelvic nodal
volumes in
endometrial
cancer adj
therapy
Anteroposterior
and lateral
separation.
BMI not available
for all pts
9 (per
Adjuvant
Brest cancer
Breast size
6
Anorectal
cancer
Gender and
location of tumor
5
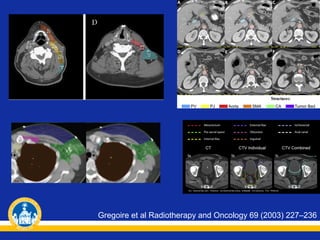
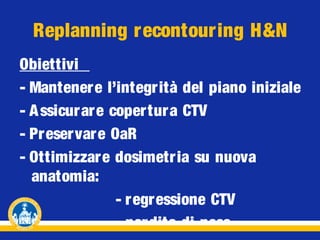
H&N nodal
level and OAR
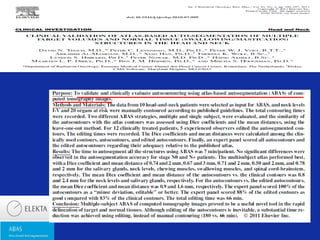
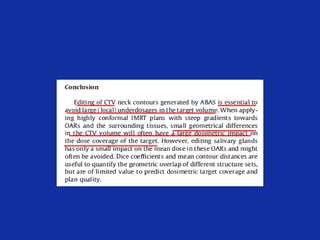
Young et al,
Int. J. Radiation
Oncology Biol.
Phys., Vol. 79, No. 3,
pp. 943–947, 2011
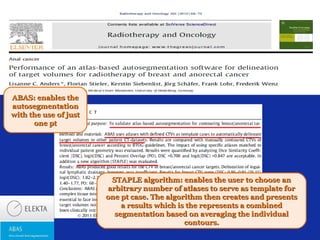
Anders et al,
Radiotherapy and
Oncology 102
(2012) 68–73
group)
Teguh et al,
Int. J. Radiation
Oncology Biol. Phys.,
Vol. 81, No. 4, pp.
950–957, 2011
Gambacorta
et al,
10
Acta Oncol. 2013
Jan 22. [Epub ahead
of print]
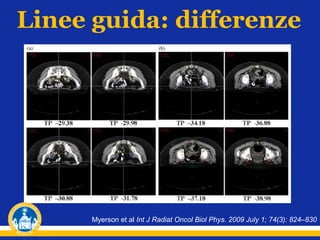
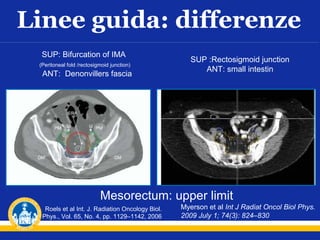
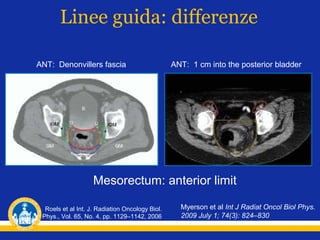
Pelvic lymph
nodes in
locally
advanced
rectal cancer
Mean Dice
coefficient
0.8
Spared
time
26%
(p<0.000001)
-
0.79-0.85
-
0.67-0.79
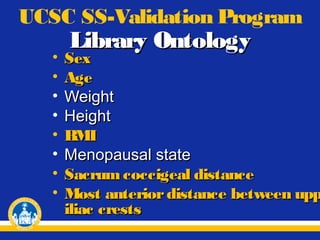
Sex, age, weight, height,
BMI, menopausal state,
sacro-cocciegeal
distance, most anterior
distance between upper
iliac crests
0.86-0.91
56%
0.70
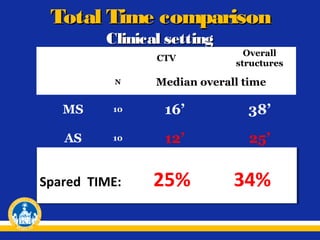
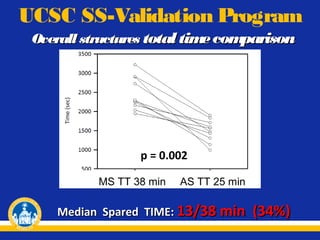
25-34%](https://image.slidesharecdn.com/dice-corso27-131015031547-phpapp01/85/Dice-corso_27-02-80-320.jpg)