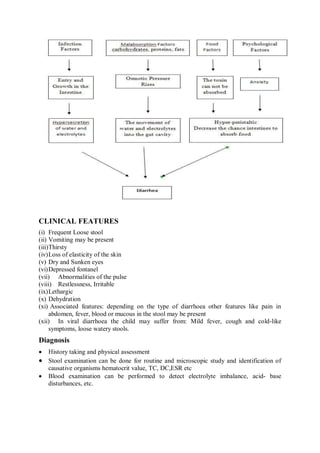
Diarrhea is common in children under 2 years old and is usually caused by viral or bacterial infections. It can lead to dehydration if fluid losses are not replaced. Dehydration is classified as none, some, or severe based on signs like thirst, skin pinch, and sunken eyes. Treatment involves oral rehydration solution to replace fluids based on the dehydration classification. For severe dehydration, IV fluids are given quickly followed by oral fluids. Preventing diarrhea involves exclusive breastfeeding, hand washing, safe water and food, and immunizations. Managing diarrhea at home includes extra fluids, continued feeding, zinc supplementation, and seeking care for danger signs.